| Total CBD: | 500 – 2500 mg |
| Potency: | 16.6 - 83.3 mg/mL |
| Cost per mg CBD: | $0.12 – $0.18 |
| Extract Type: | Full-spectrum |
| THC Content: | <0.3% |
Evidence based
CBD Oil for Seizures & Epilepsy: Benefits, Dosage, & Side Effects
Research suggests CBD is a safe and effective treatment for seizure disorders.
1 in 10 patients are seizure-free after taking CBD oil & 70% had dramatic reductions in symptoms.
Epilepsy is the fourth most common neurological disorder, according to the Epilepsy Foundation.
CBD is reported to be one of the most effective treatment options for this condition — even for types of epilepsy proven to be difficult to treat with conventional medicine.
In this article, we’ll discuss exactly how effective CBD is for treating epilepsy, which types of epilepsy CBD works best for, and how to source the right kind of CBD to use.

The Benefits of CBD Oil For Epilepsy
The benefits of CBD oil for epilepsy include:
- Alleviates convulsions
- Protects the neurons from damage
- Regulates excess brain activity
- Reduces brain inflammation
- Promotes GABA activity in the brain
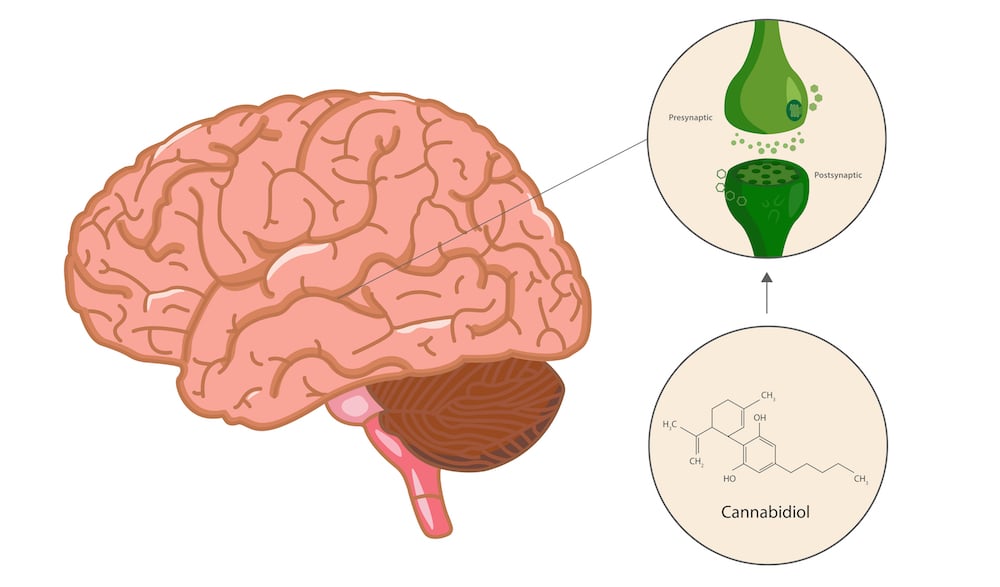
Despite all the research we have in the effects of CBD for epileptic conditions, we still don’t know the exact mechanisms involved.
Seizures are incredibly complex, and the causes generally involve multiple separate organ dysfunctions combining to produce symptoms. Therefore, deciding which part of this interaction is improved with CBD is hard to pinpoint.
Here are the current theories based on clinical, in vivo, and in vitro research findings.
1. Reduces Epileptic Convulsions
Epileptic-induced rodents were given various concentrations of CBD. The highest-dose group (100 mg per kg) showed significant improvements in muscle contractions during seizures [4].
2. Regulates Electrical Activity in The Brain
Seizures are characterized by excessive and chaotic electrical activity in the brain.
Electrical activity is largely regulated by the vanilloid receptors (TRPV).
CBD and CBDV have both been shown to regulate these vanilloid receptors (TRPV1) in the brain [1].
When TRPV1 is overactivated for any reason, it induces epileptic seizures. CBD and CBDV have been found to control the overactivity of this receptor in the brain — potentially leading to fewer seizures.
3. Protects The Brain Cells
CBD and many other cannabinoids in the cannabis plant have been shown to have broad, non-specific neuroprotective effects on the brain. Some of these neuroprotective effects are thought to be partly responsible for CBD’s powerful anti-epileptic activity.
CBD is protective for other neurological conditions, including:
- Multiple sclerosis [5]
- Alzheimer’s disease [6]
- Spinal cord injury [8]
- Prion disease (minor improvement) [9]
- Parkinson’s disease [9]
4. Inhibits Brain Inflammation
As with most neurological disorders, inflammation is a huge factor in epilepsy [10].
A lot of evidence suggests CBD is an effective anti-inflammatory compound for the brain — potentially alleviating one of the significant factors for neurological disorders such as epilepsy.
CBD is effective because its fat-soluble nature allows it to pass through the blood-brain barrier efficiently. It also offers anti-inflammatory effects through some different inflammatory messengers and immune-regulating cells [11, 12, 13].

What’s The Dose of CBD Oil For Seizures?
Figuring out the right dose of CBD for epilepsy is difficult — and will likely require some trial and error.
Everybody responds to CBD differently. Some people require high doses; others much lower. You won’t know for sure the ideal dose you need without experience.
In general, people with epilepsy require higher-than-average dosing to get the maximum amount of benefits from the compound. This is why we recommend buying a high-potency CBD oil. If you buy a low-potency CBD product and then realize you need a high dose to see any benefits, you’re likely to need to take the entire bottle for a single dose. High-potency oils last longer by delivering the same amount of CBD in a smaller amount of oil or capsules.
With that said, we recommend starting at a low dose and building up gradually over time until you reach a dose that provides the level of relief you’re looking for.
Recommended strength for epilepsy: high strength
We’ve outlined the standard dosage schedule below based on weight and strength.
To learn how to calculate these doses yourself, check out our Guide to Dosing CBD.
CBD Dosage Calculator
Tips for Getting the Most Out of CBD Supplements for Epilepsy:
- Always seek out high-quality CBD products to avoid contamination with heavy metals or pesticides — which can make epilepsy even worse
- Use full-spectrum extracts for the best results — research suggests these extracts are more effective than isolated or purified CBD products
- Increase the dose gradually — start with a low dose and build up to a higher dose until symptoms are reduced
- Combine CBD with other antiepileptic treatments and dietary changes — such as a ketogenic diet, regular exercise, and psychotherapy when appropriate
- Take CBD regularly — the effects are more pronounced after several weeks of regular use
What is Epilepsy?
Epilepsy is a spectrum of disorders involving the primary symptom: unprovoked seizures. Other health issues may or may not also be present. Everybody experiences epilepsy differently, and seizures can vary significantly in frequency and severity.
Some epileptic patients suffer from seizures one or two times per year, while others can experience nearly nonstop seizures throughout the day.
Seizures can involve whole-body convulsions (grand mal), remain confined to one limb (Jacksonian seizures), or involve lapses in consciousness (petit mal). We’ll include more on the different types of seizures later.
The seizure itself is the result of dysfunctional electrical activity in the brain — which can originate from anywhere in the brain. This abnormal electrical activity can remain confined to the area in which it started, or it can spread throughout the entire brain. In most cases, the latter is more severe.
People suffering from epilepsy usually have the condition for the rest of their life. However, it can come and go from one year to the next. Some people report being seizure-free for up to six years before having another seizure.
There are many different forms of epilepsy and numerous potential causes for each one. It can, therefore, be difficult for doctors to pinpoint the exact cause of the seizures in many cases.
Symptoms of Epilepsy
- Temporary confusion
- Prolonged staring
- Uncontrollable jerking movements
- Loss of consciousness
- A sudden sense of intense fear or anxiety
- Lapses in memory
What Causes Seizures & Epilepsy?
Seizures are the primary symptoms of epilepsy. Although epilepsy is characterized by recurring seizures, there are other causes, such as high fever or head injuries.
The brain is made up of billions of specialized cells called neurons. They’re designed to transfer messages throughout the brain and body using electrical impulses. To do this effectively, the neurons in the brain need to work together.
In the event of a seizure, large groups of neurons will send messages at the same time (hypersynchrony), disrupting normal brain function. This can cause changes in taste, vision, sound, smell, language, posture, memory, emotion, and consciousness.
Some seizures will affect the entire brain; others only specific regions. The severity of the electrical activity and how much of the brain is affected will determine the individual side-effects. Ultimately, no seizure is the same.
Causes of Seizures May Include:
- Brain injuries
- Structural abnormalities in the brain
- High fevers (children)
- Trauma
- Stroke
- Brain infection
- Brain tumor
- Low blood sugar
- Muscle disorders
There are different forms that seizures can happen depending on the individual and the type of epilepsy they have. Some people will experience one, two, or all three.
Three Types of Epilepsy
There are three different types of epilepsy.
The main differentiating factor for epilepsy is the types of seizures experienced, but there are other factors depending on the site of electrical dysfunction in the brain and the underlying cause of the condition.
Over the past decade, a group called the International League Against Epilepsy (ILAE) has been working hard to standardize the terminology used in diagnosing and describing epilepsy.
Here are the definitions listed in their 2017 outline.
1. Focal Onset
Focal onset epileptics experience abnormal electrical activity in only specific regions of the brain. They used to be called “partial seizures.”
There are four types of focal seizures:
- Focal-aware seizures — the patient is aware of the seizure while it’s taking place.
- Focal-impaired awareness seizures — the patient is unaware or unconscious during the seizure.
- Focal motor seizures — these involve movements such as rubbing hands together or twitching during the seizure.
- Focal non-motor seizures — these do not involve muscle twitches or movements, but instead shifts in thinking and emotions during the seizure. Waves of heat or cold, a racing heart, or intense emotions are common.
2. Generalized Onset
Generalized onset seizures involve abnormal electrical activity throughout both sides of the brain, resulting in widespread side effects throughout the body.
Within generalized onset epilepsies, there are two types — motor onset and non-motor onset.
Motor onset conditions used to be referred to as “grand mal” seizures — in some circles, they still are. They result in full-body seizures and an inability to control the body while the seizures are occurring. They can last anywhere from a few seconds to a few hours. CBD is useful for these types of seizures due to its ability to relax muscle contractions around the body.
Non-motor onset seizure conditions are usually called “absence” seizures. They involve periods of staring into space or repetitive movements (such as tapping hands or licking lips). These types of seizures make it seem as though the person having the seizure is no longer there — hence the name “absence seizures.”
3. Unknown Onset
As the name implies, any seizure where the source of the seizure can’t be identified is referred to as having an unknown onset. These seizures are especially challenging to treat.
Epileptic Syndromes
The new terminology outlined by the ILAE does not change the characterization of epileptic syndromes — of which there are quite a few.
The Most Common Epileptic Syndromes Include:
- Lennox-Gastaut Syndrome (LGS)
- Dravet Syndrome
- Juvenile Myoclonic Epilepsy (JME)
- Benign rolandic epilepsy (BRE)
- Childhood absence epilepsy (CAE)
- Infantile spasms (or West syndrome)
The Risks of Epilepsy
Epilepsy can endanger the safety of those affected. It can be risky to drive, work, or even cross the street. If a seizure comes on suddenly, those affected are unlikely to get out of harm’s way.
Conventional Treatment Options for Epilepsy
It’s important to remember that epilepsy is a spectrum. Certain medications or other treatment options tend to work better for some forms of epilepsy over others. In some cases, no conventional treatment works for the patient’s requirement — these are usually the people that begin using CBD.
Medications for Epilepsy Include:
- Epidolex (cannabidiol)
- Topamax (topiramate)
- Lamictal (lamotrigine)
- Klonopin (clonazepam)
- Felbatol (felbamate)
- Depakote (valproate)
- Onfi (clobazam)
- Diacomit (stiripentol)
Medical Marijuana for Epilepsy
It’s clear that marijuana is a useful supplement for different forms of epilepsy, including both generalized and focal, along with some epileptic syndromes.
Studies have shown that CBD is the active constituent of these effects. Interestingly, a meta-analysis recently showed that although any form of CBD offers benefits, a full-spectrum CBD extract containing a variety of other cannabinoids was more beneficial and had fewer side effects overall [2].
For this reason, we recommend using a quality full-spectrum product over pharmaceutical versions such as Sativex® or Epidolex®, as well as CBD products made from 99.9% pure CBD isolates.
It’s likely the other cannabinoids in the full-spectrum extracts, along with the terpenes and various other phytochemicals, work synergistically to produce the associated benefits.

The Story of Charlotte Figi
Charlotte Figi is an American girl with a severe case of Dravet syndrome who changed the way we treat epilepsy forever.
When Charlotte was just six years old, her parents signed a “do not resuscitate” order for their little girl. This meant that in the event of an emergency that saw Charlotte stop breathing or her heart stops beating, medical professionals would not be allowed to step in and save her life.
Her symptoms were very severe — she’d often experience hundreds of seizures each week. She could barely speak, and her quality of life was at an all-time low.
Even after trying numerous medications, the Figis saw virtually no improvement in their daughter’s condition.
It wasn’t until 2011 that the Figis decided to try cannabis for their daughter — and it worked.
Here seizures dropped from 1200 per month to about 3 — and the ones she had were significantly less severe. She can now talk, play, and live a life much closer to “normal.”
The media attention that followed this story exploded and is arguably the catalyst that led to the establishment of the CBD market we’re now experiencing. This is because it was discovered that CBD was the compound responsible for treating Charlotte’s condition. Researchers flocked to test it out on other types of epilepsy, as well as other medical conditions.
Guide to Using CBD for Epilepsy
CBD is becoming one of the most common treatment options for epileptics. However, with poor regulations in the CBD market, there is an alarming amount of low-quality products containing contaminants such as heavy metals or pesticides that can damage the neurons and potentially make epilepsy symptoms worse.
There are also a lot of companies selling oils with specific amounts of CBD listed on the bottle — but when tested by third parties, they’re found to contain only a fraction of the amount advertised.
When it comes to using CBD for epilepsy, it’s critical that you use only high-quality, contaminant-free, and high-potency products.
It’s also been proven through meta-analysis that a full-spectrum extract rich in CBD and other cannabinoids and terpenes has the biggest impact on epileptic conditions [2].
For this reason, we recommend searching specifically for a product with at least 50 mg per mL of CBD that is made from certified organic hemp and has publicly listed third-party test results.
How to Get a Prescription for Medical Cannabis & CBD
Although every country has its own rules regarding the use of medical marijuana, most countries with a medical program will prescribe it for epilepsy.
The National Institute of Health and Clinical Excellence is working on official guidance for prescribing medical cannabis.
Epilepsy treatment is expected to be one of the primary focus points for this piece, which is expected to be completed at the end of 2020.
If your country (or state) doesn’t have a medical marijuana program, low-THC hemp extracts are an excellent alternative. These are classified as nutritional supplements in most countries and are non-psychoactive.
Finding the Right CBD Supplements for Epilepsy
There are so many different cannabis companies selling CBD oils, capsules, and topicals — it can be hard to separate the good from the bad.
As a general guide, always look for the following:
- Products containing full-spectrum extracts
- Potencies of at least 50 mg per mL
- Productos with third-party lab tests posted
- Products made from certified organic hemp
- Extracts containing low THC (less than 0.3%)
1. CBD Oils For Epilepsy
CBD oils are the most popular form of CBD because it simplifies dosing, it can be stored for long periods of time, it is one of the cheapest forms of CBD and has high bioavailability.
2. CBD Capsules For Epilepsy
CBD capsules provide another great option for people who want a simple way to get their dose without having to measure or taste CBD oil. However, capsules are slightly more expensive on average than oils.
3. CBD Edibles For Epilepsy
Edible CBD products are also available — but aren’t recommended for daily CBD supplementation due to the high sugar content and inconsistencies with dosing. These are great for occasional use to make your CBD use more interesting (and flavorful) but not ideal for everyday use.
4. CBD Vape Oils & E-Liquids For Epilepsy
CBD vape oils and vape pens are also an option, and many people with epilepsy choose to use this method to get their dose of CBD. The benefit with vape oils is that the CBD enters the bloodstream almost immediately, offering fast relief from symptoms.
Unless vaping irritates your lungs, or you’d rather avoid it altogether, keep some vape oil on hand to address symptom flare-ups promptly without having to wait for oils or capsules to absorb through the digestive tract.
CBD & Epilepsy: What the Research Says
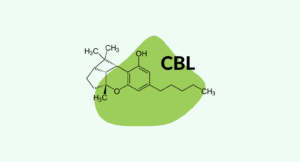
Cannabidiol (CBD) is one of over 66 different cannabinoids found in the cannabis plant.
There are two main cannabinoids in the cannabis plant that account for more than half the total cannabinoid content. CBD is non-psychoactive (meaning it won’t make you feel high). It’s also the primary ingredient responsible for the antiepileptic effects of the cannabis plant.
A pharmaceutical CBD preparation — Epidolex (cannabidiol) — was approved in 2018 for the treatment of Lennox-Gastaut syndrome (LGS) and Dravet syndrome — two forms of epilepsy known for resisting treatment.
A recent meta-analysis involving 670 people with various forms of epilepsy found that 71% of people taking CBD-rich full-spectrum extracts experienced reduced seizure frequency [2].
Roughly 40% of the people in this study had the frequency of seizures cut in half, and a quarter had an incredible 70% drop in episodes.
Amazingly, 10% of the group were reported to be seizure-free at the end of the study.
CBD works — there’s no doubt about it. The hard part now is determining exactly how it works.
We’re still uncovering exactly how CBD is useful for treating epilepsy and seizures. Even GW Pharmaceuticals admits on its website that the mechanism of action isn’t clear. GW Pharmaceuticals is the creator of Sativex® — the new cannabinoid-based pharmaceutical that’s been gaining a lot of hype lately as a breakthrough new treatment for epilepsy.
There are a few good theories, however.
Final Verdict: Can CBD Help With Epilepsy & Seizures?
CBD is perhaps one of the most exciting new treatment options for epilepsy — including epileptic syndromes such as Dravet syndrome that are problematically resistant to treatment.
To get the most out of CBD supplementation for epilepsy, a high-quality, full-spectrum extract should be used. It’s also recommended to opt for a high-potency option because, in most cases, high doses are needed to get the same level of benefits reported in the scientific literature.
Check out some of our recent reviews to vet a company and their product before you make a purchase. Remember only to buy products that are made from certified organic hemp and have been tested for purity and potency by third-party labs.
If a product doesn’t check these boxes, it’s wise to avoid taking them for epilepsy. You don’t want to make symptoms worse.
References
- Iannotti, F. A., Hill, C. L., Leo, A., Alhusaini, A., Soubrane, C., Mazzarella, E., … & Stephens, G. J. (2014). Nonpsychotropic plant cannabinoids, cannabidivarin (CBDV) and cannabidiol (CBD), activate and desensitize transient receptor potential vanilloid 1 (TRPV1) channels in vitro: potential for the treatment of neuronal hyperexcitability. ACS chemical neuroscience, 5(11), 1131-1141.
- Pamplona, F. A., daSilva, L. R., & Coan, A. C. (2018). Potential clinical benefits of CBD-rich Cannabis extracts over purified cannabidiol (CBD) in treatment-resistant epilepsy: observational data meta-analysis. Frontiers in neurology, 9, 759.
- Miller, J. W. (2011). How dangerous is epilepsy?. Epilepsy currents, 11(3), 84-85.
- Jones, N. A., Hill, A. J., Smith, I., Bevan, S. A., Williams, C. M., Whalley, B. J., & Stephens, G. J. (2010). Cannabidiol displays antiepileptiform and antiseizure properties in vitro and in vivo. Journal of Pharmacology and Experimental Therapeutics, 332(2), 569-577.
- Wade, D. T., Collin, C., Stott, C., & Duncombe, P. (2010). Meta-analysis of the efficacy and safety of Sativex (nabiximols), on spasticity in people with multiple sclerosis. Multiple Sclerosis Journal, 16(6), 707-714.
- Martín-Moreno, A. M., Reigada, D., Ramírez, B. G., Mechoulam, R., Innamorato, N., Cuadrado, A., & de Ceballos, M. L. (2011). Cannabidiol and other cannabinoids reduce microglial activation in vitro and in vivo: relevance to Alzheimers′ disease. Molecular pharmacology, mol-111.
- Barnes, M. P. (2006). Sativex®: clinical efficacy and tolerability in the treatment of symptoms of multiple sclerosis and neuropathic pain. Expert opinion on pharmacotherapy, 7(5), 607-615.
- Kwiatkoski, M., Guimaraes, F. S., & Del-Bel, E. (2012). Cannabidiol-treated rats exhibited higher motor score after cryogenic spinal cord injury. Neurotoxicity research, 21(3), 271-280.
- Dirikoc, S., Priola, S. A., Marella, M., Zsürger, N., & Chabry, J. (2007). Nonpsychoactive cannabidiol prevents prion accumulation and protects neurons against prion toxicity. Journal of Neuroscience, 27(36), 9537-9544.
- Vezzani, A., French, J., Bartfai, T., & Baram, T. Z. (2011). The role of inflammation in epilepsy. Nature reviews neurology, 7(1), 31.
- Srivastava, M. D., Srivastava, B. I. S., & Brouhard, B. (1998). Δ9 tetrahydrocannabinol and cannabidiol alter cytokine production by human immune cells. Immunopharmacology, 40(3), 179-185.
- Kozela, E., Pietr, M., Juknat, A., Rimmerman, N., Levy, R., & Vogel, Z. (2010). Cannabinoids Δ9-tetrahydrocannabinol and cannabidiol differentially inhibit the lipopolysaccharide-activated NF-κB and interferon-β/STAT proinflammatory pathways in BV-2 microglial cells. Journal of biological chemistry, 285(3), 1616-1626.
- Vuolo, F., Petronilho, F., Sonai, B., Ritter, C., Hallak, J. E., Zuardi, A. W., … & Dal-Pizzol, F. (2015). Evaluation of serum cytokines levels and the role of cannabidiol treatment in animal model of asthma. Mediators of inflammation, 2015.
More Health Conditions to Explore
-
Conditions Related to Health Benefits
- CBD For Allergies: Can This Cannabinoid Ease Symptoms?
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- CBD For Psoriasis: Can CBD Help to Alleviate Symptoms?
- Traumatic Brain Injury (TBI)
- Arthritis
- Anxiety & Depression
- Weight Loss
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Antibiotic Resistance
- Asthma
- Atherosclerosis
- Autism
- Acne
- Bipolar Disorder
- Pain
- Crohn's Disease & Ulcerative Colitis
- Diabetes
- Epilepsy
- Endocrine Disorders
- Fibromyalgia
- Fatty Liver Disease
- Glaucoma
- Hypertension
- Heart Disease
- Huntington's Disease
- Inflammation
- Irritable Bowel Syndrome (IBS)
- Kidney Disease
- Migraine Headaches
- Muscle Recovery
- Multiple Sclerosis
- Motion Sickness
- Metabolic Syndrome
- Neurodegeneration
- Cancer
- Nausea
- Neuropathic (Nerve) Pain
- Osteoporosis/Bone Health
- Obsessive-Compulsive Disorder (OCD)
- Polycystic Ovarian Syndrome (PCOS)
- PTSD
- Prion/Mad Cow Disease
- Premenstrual Syndrome (PMS)
- Parkinson’s Disease
- Schizophrenia
- Sickle Cell Anemia
- Stroke
-
Conditions Related to Products
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 10 CBD Oils For Back Pain
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Terpene Concentrates
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- Best Dry Herb Vaporizers
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
Conditions Related to Topicals
-
Conditions Related to Oils & Tinctures
-
Conditions Related to Edibles
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Honey
- CBD Chewing Gum
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Coffee
- CBD Drinks & Shots
- CBD Capsules
-
Conditions Related to Gummies
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
-
Conditions Related to Hemp Flower
-
-
Conditions Related to Terpenes
-
-
Conditions Related to Cultivation
-
Conditions Related to Concentrates
-
Conditions Related to Delta 8 THC
-
Conditions Related to Delta 9 THC
-
-
-
-
Conditions Related to CBD
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
-
Conditions Related to THC-O
-
-
Conditions Related to Joint Health
-
Conditions Related to Pain Disorders
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Traumatic Brain Injury (TBI)
- Arthritis
- Pain
- Fibromyalgia
- Glaucoma
- Inflammation
- Kidney Disease
- Migraine Headaches
- Multiple Sclerosis
- Neuropathic (Nerve) Pain
- Premenstrual Syndrome (PMS)
- Sickle Cell Anemia
-
Conditions Related to Autoimmune Disease
-
Conditions Related to Cognitive Health
-
Conditions Related to Metabolic Disorders
-
Conditions Related to Psychological Disorders
-
Conditions Related to Muscles & Bones
-
Conditions Related to Nervous System
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- Traumatic Brain Injury (TBI)
- Anxiety & Depression
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Autism
- Bipolar Disorder
- Epilepsy
- Huntington's Disease
- Inflammation
- Migraine Headaches
- Multiple Sclerosis
- Motion Sickness
- Neurodegeneration
- Neuropathic (Nerve) Pain
- Obsessive-Compulsive Disorder (OCD)
- PTSD
- Prion/Mad Cow Disease
- Parkinson’s Disease
- Schizophrenia
-
-
Conditions Related to Reproductive Health
-
Conditions Related to Hormones & Endocrine
-
Conditions Related to Skin Health
-
Conditions Related to Cardiovascular System
-
Conditions Related to Digestive System
-
Conditions Related to Genetic Disorders
-
Conditions Related to For Children