| Total CBD: | 500 – 2500 mg |
| Potency: | 16.6 - 83.3 mg/mL |
| Cost per mg CBD: | $0.12 – $0.18 |
| Extract Type: | Full-spectrum |
| THC Content: | <0.3% |
Evidence based
CBD for IBS: Everything You Need to Know
IBS is frustrating. There are few effective treatments for the condition, which can make it hard to live your life to the fullest.
Here’s how CBD might be able to help.
Irritable bowel syndrome (IBS) is not life-threatening, but it can severely disrupt the quality of life for those affected.
Roughly 1 out of 10 people in the developed world have symptoms consistent with IBS [3].
Despite how common the condition is, IBS is not well understood. As a result, there are few effective treatment options available aside from managing symptoms.
Here we’ll go over how CBD may be used to support an IBS diagnosis, how to use it, what its limitations are, and how to get the most out of it with other diet and lifestyld modifications.
Best CBD Oils For IBS
- Royal CBD Oil — Best CBD Oil For IBS Overall
- Gold Bee CBD Oil — Best Organic CBD Oil
- Phoria CBD Oil With Curcumin — CBD & Turmeric
The Benefits of CBD Oil For IBS
There are many potential causes for IBS, but much of what triggers the condition remains unknown. Most of the causes point to a loss of equilibrium in the digestive tract. So the carefully orchestrated balance involved with digestion, absorption, immune defense, and excretion is compromised.
Cannabidiol (CBD) helps with this problem because it serves as a way to “calibrate” different parts of the body. It does this by improving the communication between cells through the endocannabinoid system.

The benefits of CBD oil for IBS Include:
- Addresses anandamide deficiencies [13]
- Reduces inflammation [7, 8]
- Inhibits digestive muscle hyperactivity and cramping [5, 6]
- Decreases appetite [9]
CBD will affect the condition differently depending on the form of IBS.
People who have IBS with diarrhea (IBS-D) are likely to experience the most benefit from CBD because cannabis slows muscle contraction in the digestive tract.
But people who have IBS with constipation (IBS-C) can still find benefit from CBD due to the anti-inflammatory, appetite-suppressant, and immune-stimulating properties of the compound.
We’ll get into the different forms of IBS and how CBD is used to support them later on.
What Form of CBD Should I Use?
CBD comes in all different forms. You can buy oils, capsules and concentrates.
When it comes to IBS, the most popular options are oils, capsules, and suppositories.
CBD oils and capsules are easy to take, to store for long periods of time, and can be accurately dosed.
Suppositories have the benefit of delivering the CBD directly to the affected area. This is best for severe IBS-D (more on this below) but can benefit other forms of IBS as well.
What’s The Dose of CBD Oil For IBS?
Dosing CBD can be a challenge because it affects everybody differently.
Some people take 50 mg of CBD per day, while others need more or less.
The dose also depends on the form of CBD you’re taking. As we mentioned, CBD oil and suppositories are the most popular for people with IBS, but the dose for each form varies significantly.
If using oils or capsules, the best way to find a good starting dose it to read through our CBD oil dosing guide.
CBD Dosage Calculator
For IBS, we recommend starting at the low strength and working your way up slowly to see how you react to CBD.
It will likely take about two or three weeks of regular CBD use before you start noticing any real benefits for your IBS symptoms.
If using CBD suppositories, it’s best to follow the specific instructions listed by the supplier on the packaging. Concentrations can vary from one CBD suppository to the next.
How to Get the Most Out of CBD Oil for IBS
CBD shouldn’t be used alone to treat IBS. This condition is highly complex and involves multiple organ systems.
Other forms of treatment, including dietary changes and physical activity, are essential. If these lifestyle changes aren’t addressed, CBD is not likely to have any effect at all.
You can think of CBD as a bus driver — it will drive the occupants towards a destination, but they can’t arrive without a well-maintained bus filled with gas.
CBD is a tool to help alleviate uncomfortable symptoms of IBS and is used to bring the body back to balance.
What is CBD Oil?
CBD stands for cannabidiol. It’s one of the primary cannabinoids in the cannabis plant.
Most CBD oils on the market today come from the hemp plant (Cannabis sativa), which is a strain of cannabis naturally low on THC — the primary psychoactive cannabinoid.
This means that most CBD products on the market have no psychoactive effects.

CBD is used as a health supplement for a wide range of medical conditions. It owes much of its ability to support health to its involvement with the endocannabinoid system.
The endocannabinoid system regulates balance in the body, otherwise known as homeostasis. This includes the immune, digestive, neurological, musculoskeletal, and integumentary (skin) systems.
What is Irritable Bowel Syndrome?
Irritable bowel syndrome (or IBS) is classified as a syndrome, rather than a disease because it’s a set of symptoms that can’t be linked to a particular cause.
IBS can be summarized as a “widespread dysfunction of the digestive tract.”
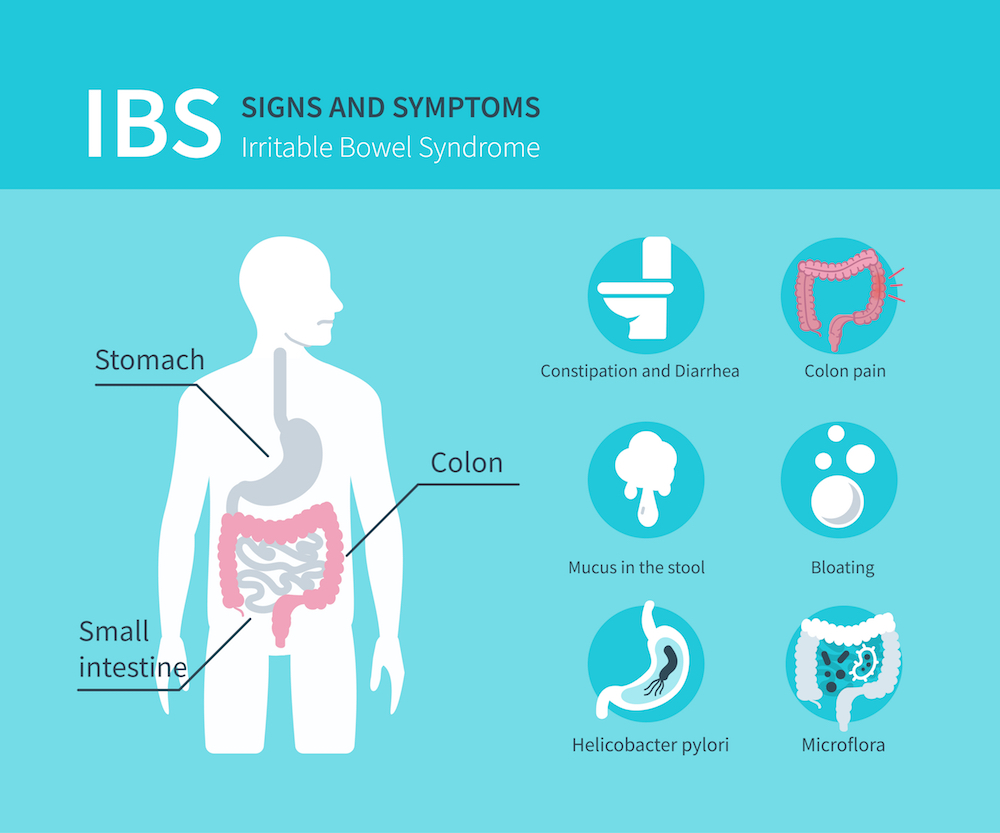
Symptoms involve bloating, abdominal pain, indigestion, and changes in bowel movements (constipation or diarrhea, which can be severe).
The symptoms of IBS are very similar to those of inflammatory bowel disease (IBD). The difference is that IBD has inflammation present in the gastrointestinal tract, confirmed by Lab tests and special cameras inserted in the digestive system.
If no inflammation is present to confirm a diagnosis of IBD, an IBS diagnosis is given instead.
In this process, there are some diagnostic criteria put in place by various experts, but none of them are conclusive and not all doctors agree on them for a diagnosis of IBS.
The most popular criteria doctors tend to use is something called the Rome III Criteria.
IBS Diagnosis: The Rome III Criteria Checklist
In order to meet a diagnosis of IBS, the patient must have the following symptoms:
- Recurrent abdominal pain or discomfort at least 3 days per month over 3 months
- Symptoms involving at least two of the following characteristics:
- Improvement of symptoms with defecation
- Onset associated with a change in stool frequency
- Onset associated with a change in stool form
If these criteria are met and there is no other explanation for a cause (such as inflammation, traumatic damage, or infectious disease) the patient is diagnosed with IBS.
Symptoms of Irritable Bowel Syndrome:
- Nausea
- Abdominal pain
- Gas
- Bloating
- Feelings of “fullness”
- Constipation/Diarrhea
- Mucus in the stool
- Uncontrollable urgency to have a bowel movement
- Fatigue
- Weight gain/loss
3 Types of IBS & the Effects of CBD
20-50% of visits to a gastroenterologist end in a diagnosis of IBS [3], making it the most common functional disorder of the digestive system.
Gastroenterologists further classify IBS according to the most predominant symptoms:
1. Diarrhea-Dominant IBS (IBS-D)
This refers to IBS presented primarily with diarrhea.
IBS-D symptoms indicate that the bowels are filling with water. Common precursors for this include high sodium foods, a poor gut membrane, and hyperactive muscle activity in the digestive tract.
With high sodium foods and poor membrane control, water begins to accumulate in the areas filled with salty foods. This happens because of a principle in biophysics called osmosis: the water goes where the salt is. As the intestines fill up with water, it causes diarrhea.
Additionally, many people with IBS-D experience hyperactive muscle activity in the intestinal tract. When the muscles become spastic, they experience cramping, abdominal pain, and bloating. The digestive tract pushes food through too quickly without properly breaking it down and absorbing it. Instead, unabsorbed foods begin to ferment in the large intestine, causing severe bloating, nausea, and diarrhea.
CBD is useful for this type of IBS because it can reduce spastic muscle activity in the gut, allowing it to properly digest and absorb nutrients. For this type of IBS, it’s best to combine CBD with a low-sodium diet and a good source of soluble fiber.
2. Constipation-Dominant IBS (IBS-C)
IBS-C stands for IBS presented predominantly with constipation.
This type of IBS indicates low activity in the digestive tract. Pancreatic enzymes, bile, and stomach acid are scant. These enzymes help break down our food and stimulate the smooth muscle lining our intestines. This stimulation causes the muscles to expand and contract, moving food along the digestive tract.
If there is a problem with the secretion of digestive enzymes or muscle movement in the intestinal tract, we become constipated.
This can be extremely uncomfortable, causing symptoms such as severe bloating, feelings of fullness, nausea, fatigue, and physical belly distention.
Although nothing will produce the same level of benefit as a change in the diet, CBD does offer some unique benefits to this form of IBS.
CBD increases anandamide — a naturally occurring endocannabinoid responsible for slowing bowel movement, fighting inflammation, and controlling microbiome diversity.
3. Alternating IBS (IBS-A) or Mixed-type IBS (IBS-M)
This form of IBS involves alternating bouts of diarrhea and constipation.
The potential causes of this type of IBS are far more variable and can involve factors of both. For several months, the patient may suffer from constant diarrhea, followed by several months of severe constipation. The sudden changes in bowel activity can be due to dietary, neurological, or immunological factors — making the cause hard to isolate and treat.
CBD is useful for this type of IBS because it doesn’t push the digestive function in any specific direction. Instead, it improves the body’s ability to regulate homeostasis. Along with other therapies to manage symptoms, the body has a better chance of returning to a higher state of health on its own.
What Causes IBS?
The exact cause of IBS is not yet understood — but there are some well-accepted theories in the medical community.
Suspected Causes of IBS Include:
1. Diet
Western countries including Canada, The United States, and Sweden have the highest rates of IBS in the world [11, 12]. In the United States, roughly 1 in 10 people suffer from IBS.
These nations often consume diets high in processed foods. Foods that have been highly processed tend to have poor nutritional content (in terms of vitamins, antioxidants, minerals) and are high in calories (in the form of fat or sugar).

When we eat these foods, they tend to move slowly through our digestive tract due to the lack of fiber and bulk of the food.
The slow movement and high sugar content cause this food to ferment in the digestive tract by bacteria living there. Fermentation in this context is bad for our digestive functioning — it causes bloating, pain, and changes in bowel movements.
One of the main dietary treatments for IBS is called a low FODMAPS diet, which substitutes highly processed foods for high-fiber, low sugar ones.
Frequent fermentation of processed sugars can damage the structural integrity of the digestive lining over time — leading to accumulation of fluid and diarrhea (IBS-D) or lack of movement in the muscles in the small and large intestines causing constipation (IBS-C).
2. Viral Infection
Viral infections can cause a lot of damage to the body. Many people report their IBS symptoms started shortly after getting a stomach bug overseas. After a few days of illness, they seemed to be getting better, but their gut never fully recovered.
Viruses disrupt normal cellular function, hijacking our cells to manufacture more viruses and preventing them from their job. They can wreak havoc on an entire organ in a short amount of time.
The digestive lining is home to a complex ecosystem of bacteria and fungal species called the microbiome. The microbiome is heavily involved with digestion and absorption in the digestive tract. When we fall ill with a virus, this can cause dramatic changes to the microbiome, leaving us with long-lasting side-effects, such as IBS.
3. Neurological Dysfunction
The movement of the intestinal tract (called peristalsis) is a complex orchestra of muscle contractions working together to move food through the intestinal tract. This involves careful innervation both locally and in collaboration with the brain.
Many people find that when they drink coffee, it stimulates a bowel movement. This is a good visualization of how the nervous system affects the digestive tract.
If our nervous system is in a state of constant stimulation, we are likely to develop diarrhea (IBS-D).
If we experience the opposite (insufficient stimulation), we are likely to end up with constipation (IBS-C).
Based on neurological activity, we can compare IBS types with other side-effects that often affect IBS patients at the same time.
Neurological Characteristics of IBS and Related Side-Effects:
| IBS type | Nervous System Activity | Related Side-Effects |
| IBS-D | Too stimulated | Anxiety Panic disorders Insomnia Heart palpitations |
| IBS-C | Not stimulated enough | Fatigue Depression |
| IBS-A | Either too stimulated or not enough | Anxiety Panic disorders Insomnia Heart palpitations Fatigue Depression Immune deficiencies |
4. Inflammation
Although IBS by definition does not require visible or detectable inflammation, numerous studies have shown that IBS sufferers have low-grade inflammation of the gut wall [2]. This inflammation may be too subtle to be picked up by blood tests or visual inspection with colonoscopies/endoscopies.
Common Medications Used to Treat IBS
Lifestyle and diet changes will have the most impact on treating IBS. Besides the low FODMAP diet, it can help to reduce stress and get more exercise.
In some cases, medications can be prescribed to help reduce the symptoms of IBS. For diarrhea, drugs like loperamide, rifaximin, or eluxadoline may help. Fiber supplements, laxatives, lubiprostone, or linaclotide can be used to treat constipation. Abdominal pain can be relieved with antispasmodics. Sometimes antidepressants are prescribed for those with more extreme cases.
Suggested Reading: Is CBD Oil Safe to Use With My Medication?
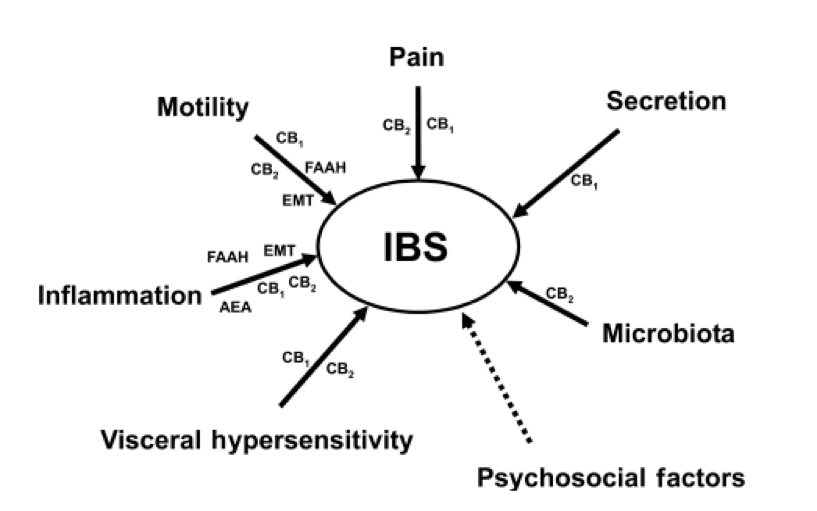
The Endocannabinoid System & IBS
The endocannabinoid system is thought to play a major role in IBS [10].
The CB1 and CB2 endocannabinoid receptors are used to regulate different processes in the human body — many of which are present in the digestive tract.
CBD for Other Functional Disorders
IBS is considered a functional disorder, suggesting there’s a clear problem with the function of the organ without an apparent cause.
Other conditions that fit this category are fibromyalgia and chronic fatigue syndrome — both of which are also improved with regular CBD use. The mysterious nature of these conditions makes it difficult to pinpoint exactly why CBD is so useful for treating them, but the likely explanation is the role CBD plays in homeostasis.
Homeostasis is the state of balance in the body. It penetrates virtually every aspect of life — from body temperature to digestive enzyme secretion. Any issues with homeostasis can negatively affect our health.
CBD serves as a useful tool for regulating homeostasis, which is why this compound has so many different benefits.
Key Takeaways: Using CBD for IBS
Although IBS isn’t well understood, it likely involves a combined dysfunction of multiple organ systems, lifestyle habits, and diet — CBD offers broad benefits towards different variations of the condition.
It’s best to use CBD in the form of an oil, capsule, or suppository for optimal results. It’s also important to take CBD oil for long periods of time to exert its full effects. CBD can take a while to start providing benefits for this condition because there are many factors involved.
Through persistent CBD supplementation, dietary and lifestyle changes, and patience, IBS symptoms can be forced into remission for long periods of time.
References Cited in This Article
- Russo, E. B. (2008). Clinical endocannabinoid deficiency (CECD): can this concept explain therapeutic benefits of cannabis in migraine, fibromyalgia, irritable bowel syndrome and other treatment-resistant conditions?. Neuroendocrinology letters, 29(2), 192-200.
- Sinagra, E., Pompei, G., Tomasello, G., Cappello, F., Morreale, G. C., Amvrosiadis, G., … & Raimondo, D. (2016). Inflammation in irritable bowel syndrome: Myth or new treatment target?. World journal of gastroenterology, 22(7), 2242.
- Stamboldjiev, T. (2011). Management of Irritable Bowel Syndrome in Primary Care: the results of an exploratory randomised controlled trial of mebeverine, methylcellulose, placebo and a self-management website. BMC-series journals.
- Saito, Y. A., Schoenfeld, P., & Locke III, G. R. (2002). The epidemiology of irritable bowel syndrome in North America: a systematic review. The American journal of gastroenterology, 97(8), 1910-1915.
- Pertwee, R. G. (2001). Cannabinoids and the gastrointestinal tract. Gut, 48(6), 859-867.
- Hornby, P. J., & Prouty, S. M. (2004). Involvement of cannabinoid receptors in gut motility and visceral perception. British journal of pharmacology, 141(8), 1335-1345.
- Ribeiro, A., Ferraz-de-Paula, V., Pinheiro, M. L., Vitoretti, L. B., Mariano-Souza, D. P., Quinteiro-Filho, W. M., … & Hallak, J. E. (2012). Cannabidiol, a non-psychotropic plant-derived cannabinoid, decreases inflammation in a murine model of acute lung injury: Role for the adenosine A2A receptor. European journal of pharmacology, 678(1-3), 78-85.
- De Petrocellis, L., Orlando, P., Moriello, A. S., Aviello, G., Stott, C., Izzo, A. A., & Di Marzo, V. (2012). Cannabinoid actions at TRPV channels: effects on TRPV3 and TRPV4 and their potential relevance to gastrointestinal inflammation. Acta physiologica, 204(2), 255-266.
- Mechoulam, R., & Hanus, L. (2001). The cannabinoids: an overview. Therapeutic implications in vomiting and nausea after cancer chemotherapy, in appetite promotion, in multiple sclerosis and in neuroprotection. Pain Research and Management, 6(2), 67-73.
- Storr, M. A., Yüce, B., Andrews, C. N., & Sharkey, K. A. (2008). The role of the endocannabinoid system in the pathophysiology and treatment of irritable bowel syndrome. Neurogastroenterology & Motility, 20(8), 857-868.
- Sperber, A. D., Dumitrascu, D., Fukudo, S., Gerson, C., Ghoshal, U. C., Gwee, K. A., … & Bolotin, A. (2017). The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a Rome Foundation working team literature review. Gut, 66(6), 1075-1082.
- Lovell, R. M., & Ford, A. C. (2012). Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clinical gastroenterology and hepatology, 10(7), 712-721.
- Russo, E. B. (2016). Clinical endocannabinoid deficiency reconsidered: current research supports the theory in migraine, fibromyalgia, irritable bowel, and other treatment-resistant syndromes. Cannabis and cannabinoid research, 1(1), 154-165.
- EB Russo – Cannabis and cannabinoid research, 2016. Cannabis and cannabinoid research, 1(1), 154-165.
More Health Benefits to Explore
-
Conditions Related to Health Benefits
- CBD For Allergies: Can This Cannabinoid Ease Symptoms?
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- CBD For Psoriasis: Can CBD Help to Alleviate Symptoms?
- Traumatic Brain Injury (TBI)
- Arthritis
- Anxiety & Depression
- Weight Loss
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Antibiotic Resistance
- Asthma
- Atherosclerosis
- Autism
- Acne
- Bipolar Disorder
- Pain
- Crohn's Disease & Ulcerative Colitis
- Diabetes
- Epilepsy
- Endocrine Disorders
- Fibromyalgia
- Fatty Liver Disease
- Glaucoma
- Hypertension
- Heart Disease
- Huntington's Disease
- Inflammation
- Irritable Bowel Syndrome (IBS)
- Kidney Disease
- Migraine Headaches
- Muscle Recovery
- Multiple Sclerosis
- Motion Sickness
- Metabolic Syndrome
- Neurodegeneration
- Cancer
- Nausea
- Neuropathic (Nerve) Pain
- Osteoporosis/Bone Health
- Obsessive-Compulsive Disorder (OCD)
- Polycystic Ovarian Syndrome (PCOS)
- PTSD
- Prion/Mad Cow Disease
- Premenstrual Syndrome (PMS)
- Parkinson’s Disease
- Schizophrenia
- Sickle Cell Anemia
- Stroke
-
Conditions Related to Products
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 10 CBD Oils For Back Pain
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Terpene Concentrates
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- Best Dry Herb Vaporizers
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
Conditions Related to Topicals
-
Conditions Related to Oils & Tinctures
-
Conditions Related to Edibles
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Honey
- CBD Chewing Gum
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Coffee
- CBD Drinks & Shots
- CBD Capsules
-
Conditions Related to Gummies
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
-
Conditions Related to Hemp Flower
-
-
Conditions Related to Terpenes
-
-
Conditions Related to Cultivation
-
Conditions Related to Concentrates
-
Conditions Related to Delta 8 THC
-
Conditions Related to Delta 9 THC
-
-
-
-
Conditions Related to CBD
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
-
Conditions Related to THC-O
-
-
Conditions Related to Joint Health
-
Conditions Related to Pain Disorders
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Traumatic Brain Injury (TBI)
- Arthritis
- Pain
- Fibromyalgia
- Glaucoma
- Inflammation
- Kidney Disease
- Migraine Headaches
- Multiple Sclerosis
- Neuropathic (Nerve) Pain
- Premenstrual Syndrome (PMS)
- Sickle Cell Anemia
-
Conditions Related to Autoimmune Disease
-
Conditions Related to Cognitive Health
-
Conditions Related to Metabolic Disorders
-
Conditions Related to Psychological Disorders
-
Conditions Related to Muscles & Bones
-
Conditions Related to Nervous System
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- Traumatic Brain Injury (TBI)
- Anxiety & Depression
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Autism
- Bipolar Disorder
- Epilepsy
- Huntington's Disease
- Inflammation
- Migraine Headaches
- Multiple Sclerosis
- Motion Sickness
- Neurodegeneration
- Neuropathic (Nerve) Pain
- Obsessive-Compulsive Disorder (OCD)
- PTSD
- Prion/Mad Cow Disease
- Parkinson’s Disease
- Schizophrenia
-
-
Conditions Related to Reproductive Health
-
Conditions Related to Hormones & Endocrine
-
Conditions Related to Skin Health
-
Conditions Related to Cardiovascular System
-
Conditions Related to Digestive System
-
Conditions Related to Genetic Disorders
-
Conditions Related to For Children