Evidence based
TRP Channels: What Are They & What’s Their Connection to Cannabinoids?
TRP is the other target network for cannabinoids that nobody’s talking about.
Cannabinoids primarily interact with the endocannabinoid system, but there’s evidence they activate TRP channels — just another one of the many ways they could impact our health.
What exactly are TRP channels, and where do cannabinoids fit into this?
Here’s a summary of everything you need to know about TRP Channels and the role it plays in regulating our health and resilience.
What Are TRP Channels?
Transient receptor potential (TRP) channels are mostly on the plasma membrane of many animal tissue cells and influence cellular transcription, translation, contraction, and migration [1].
These channels are susceptible to activation and inhibition from many things outside the cell, often by multiple, unrelated triggers at once [2]. Stimuli like light, touch, chemicals, temperatures, pH, and osmolarity activate these channels and then convert these signals into physiological and pathological responses.
They contribute to several diseases, including cardiovascular, neurological, metabolic, and neoplastic disorders, making them a target for diagnosis and therapy [3,4].
TRP Subfamilies
There are 28 cation permeable channels, and these are grouped into six subfamilies.
1. TRPV Channels
The transient receptor potential vanilloid (TRPV) family, including isoforms TRPV1, TRPV2, TRPV3, TRPV4, TRPM8, detect temperatures, thermal stimuli, and chemical agents (capsaicin, camphor, menthol, etc.) [5].
TRPV1 is a target for pain and inflammation relief. Block it, and you’ll block the pain from heat, cold, chemicals, and more. That’s not always good to do.
2. TRPC Channels
The transient receptor potential canonical (TRPC) family helps regulate the migration and invasion of cells. They’re seen in multiple physiological processes, such as neurotransmission, neurodevelopment, calcium signaling, kidney function, cardiovascular function, and immune response [6].
Fun fact: there’s an odd member in its group. There are seven isoforms, but only six are functional. In humans, TRPC2 is a pseudogene, which is exactly what it sounds like: a gene, but not quite. It’s there, standing in the corner, watching the others fulfill their purpose — cue flashbacks to junior high dances.
In other animals, it’s found in tissues in the vomeronasal organ (VNO), testis, spleen, and liver.
3. TRPM Channels
The transient receptor potential melastatin (TRPM) family is the most mysterious out of them all. These channels seem to help with cellular proliferation, sensing temperature, vascular development, cancer progression, and neurological diseases [7].
TRPM8 is found in neurons that sense pain and temperature and is activated by certain plant odorants like linalool and geraniol. Applying menthol and similar compounds cause TRPM8 currents [8].
4. TRPA Channels
There’s only one transient receptor potential ankyrin (TRPA) channel in humans: TRPA1. It used to be called ANKTM1 because it has many N-terminal ankyrin repeats [9].
It’s associated with thermo and mechanosensations — a fancy way of saying they sense temperatures, touch, movement, sound, and pain.
The most interesting thing about TRPA1 is that it’s chemically activated by THC [10]. Other things activate it, such as environmental irritants and “pungent compounds” like certain ingredients in wasabi, horseradish, mustard, garlic, cinnamon oil, and tear gas.
5. TRPP Channels
The transient receptor potential polycystic (TRPP) group has a lot of physiological and pathophysiological processes, making it crucial to understand [11]. TRPPs consist of integral membrane proteins that can cause autosomal dominant polycystic kidney disease (ADPKD).
TRPP1 is involved in receptor signaling and cell adhesion but doesn’t have the structure of typical TRP channels, so it was renamed Polycystin1 (PC1).
Two members, PKD1L3 and PKD2L1, play a role in taste receptor cells [12]. TRPP3 and TRPP5 are elusive, and, well, we don’t really know what they do.
6. TRPML Channels
The transient receptor potential mucolipin (TRPML) group is the smallest with only three cation channels and is found in intracellular compartments instead of plasma membranes, like the others.
TRPML2 and three aren’t linked to any human diseases and are studied less because of it. However, TRPML1 is involved in membrane trafficking, signal transduction, and LEL (late endosomes and lysosomes) ion homeostasis. Mutations cause autosomal-recessive lysosomal storage disease (LSD).
It’s a target for delaying the neurodegeneration caused by some lysosome-related diseases [13].
TRP Channels & Disease
It seems some diseases are due to TRP channels that don’t function properly [14]. This makes sense since they’re a crucial part of many biological processes.
Here are a few areas TRPs influence:
- Pain
- Thermoregulation
- Salivary fluid secretion
- Inflammation
- Cardiovascular system regulation
- Smooth muscle tone
- Lysosomal functions
Genetic Disorders
Deficits in TRP channel genes are linked to several genetic disorders [5].
- TRPC6 is linked to a kidney disease called focal and segmental glomerulosclerosis (FSGS).
- TRPV4 mutations are found in people with some neurodegenerative disorders like Charcot–Marie–Tooth disease type 2C (CMT2C).
- Certain mutations of TRPV3 cause Olmsted syndrome.
- TRPA1 mutations can cause familial episodic pain syndrome (FEPS) and defects in hot and cold sensations.
- TRPML1 mutations are found in those with autosomal-recessive lysosomal storage disease (LSD), a disorder that causes cognitive impairment and compromised motor skills.
Acquired Disease
TRPs are abundant in the brain, and their activation displays obvious effects in the central nervous system. However, TRPs are implicated in many diseases, especially hereditary [5].
- Ischemic stroke (TRPC1, TRPC4, and TRPC5 activation; TRPC6 causes positive effects)
- Analgesic potential for treating ocular pain, inflammatory pain, osteoarthritis, and neuropathic pain, among others (TRPV1, TRPV3, TRPA1, and TRPM8)
- Found in nociceptive neurons and skin tissue and play a role in itching sensations (TRPA1, TRPV1, TRPV3, and TRPV4)
- Found in smooth muscle and contribute to vascular problems (TRPV1, TRPV4, TRPC6, TRPM4)
- Chronic asthma and chronic obstructive pulmonary disease (TRPA1)
- Asthma and chronic cough (TRPV1)
- Lower urinary tract disorders, urinary incontinence, and bladder pain (TRPV1, TRPV2, TRPV4, TRPM4, TRPM8, and TRPA1)
- Diabetes (TRPV1 and TRPA1)
This is just the beginning of what research shows but gives you a good idea of the kind of impact they have.
What Are Cannabinoids?
Cannabinoids are part of the endocannabinoid system (ECS); the other two parts are enzymes and receptors. The human body makes cannabinoids (called endocannabinoids), but Cannabis makes them, too (called phytocannabinoids).
These cannabinoids interact with the receptors. There are two kinds of these (maybe three, but we don’t know for sure, so we’ll stick with two) referred to as CB1 and CB2. CB1 receptors are mostly in the central nervous system (CNS), while CB2 receptors are primarily in the immune system.
These receptors play an important role in our overall health [15]. Cannabinoids activate or inhibit these receptors, telling them to send signals and making the body respond accordingly.
The endocannabinoid system pretty much balances everything, and these cannabinoids affect its role.
Just how much impact they have is still up in the air, but we do know some can relieve pain, improve mood, and make you feel out of this world (thanks, THC).
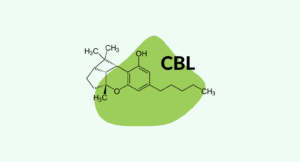
Common Cannabinoids
There are possibly more than 100 different cannabinoids in Cannabis, and most aren’t psychoactive. Few studies were done on them until recently because they didn’t seem to do anything. Now we see how faulty that assumption was and research them with a frenzy. The medicinal possibilities with these cannabinoids seem almost endless [16,17].
We don’t have time to cover every cannabinoid, but here are the most popular. Remember, this is just the tip of the iceberg.
CBD (Cannabidiol)
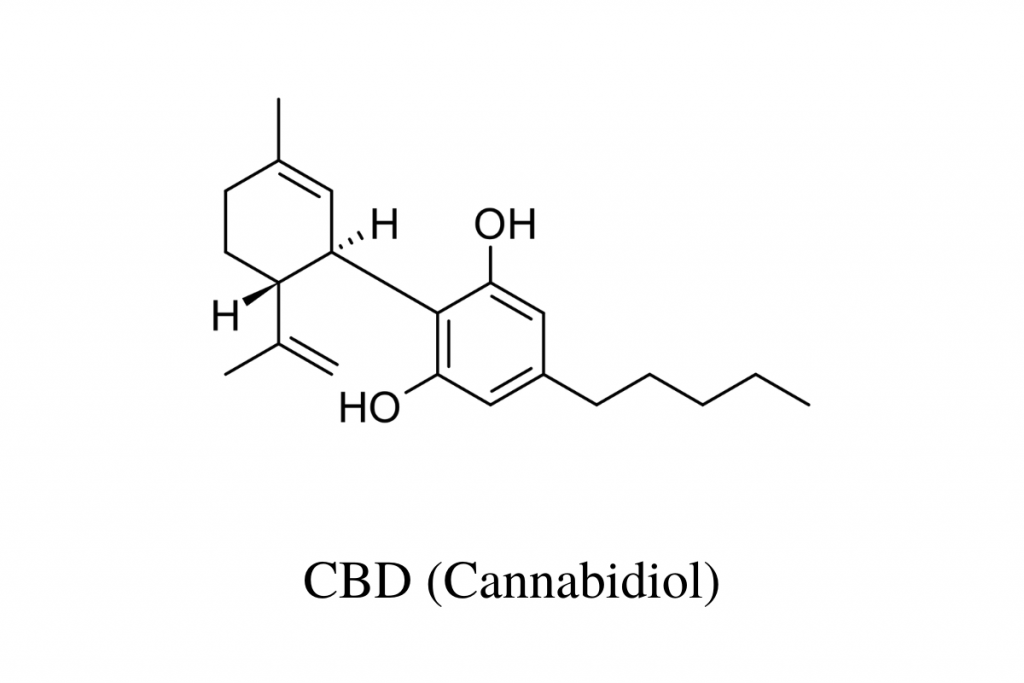
Good old CBD (cannabidiol). This one kind of kickstarted the movement and made cannabis products more mainstream and “acceptable.” Instead of a “fringe of society” thing, it became more of a “soccer mom” thing. (Note: We love all people, so don’t get offended if you fall into either group. It is what it is.)
People of all kinds use it to relieve pain and stress, and even the FDA is on board with it as an anti-seizure med [18].
THC (Delta 9-Tetrahydrocannabinol)
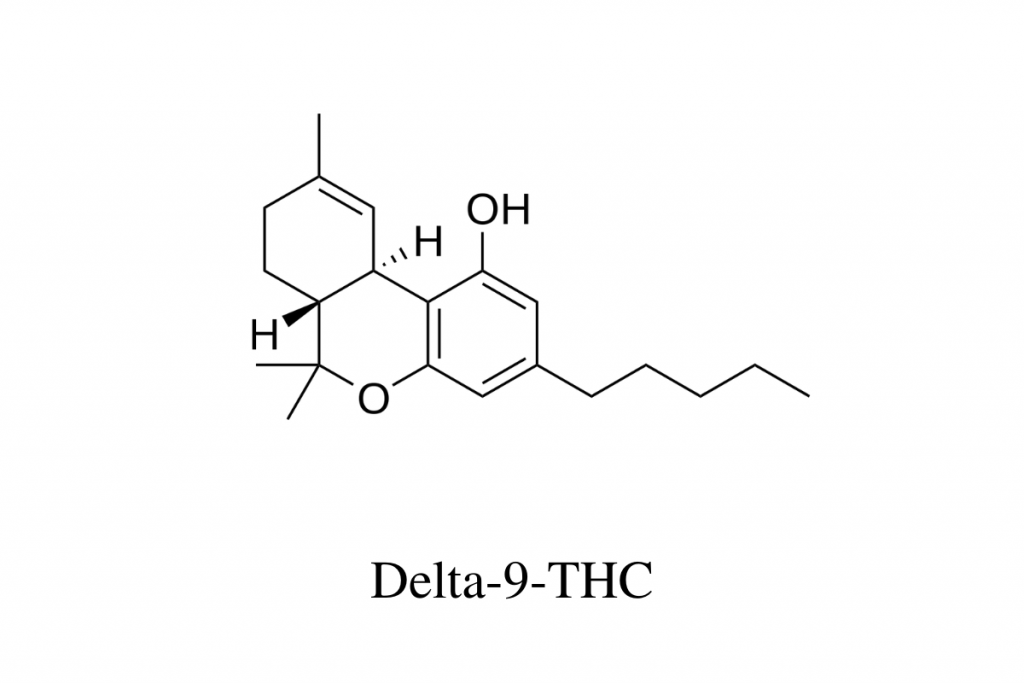
Delta 9 THC is the reason weed makes you high. It’s also a large source of its medicinal properties, though we have to credit the other cannabinoids for having its back. The entourage effect is a real thing, and they all play a role in how Cannabis makes you feel.
CBG (Cannabigerol)
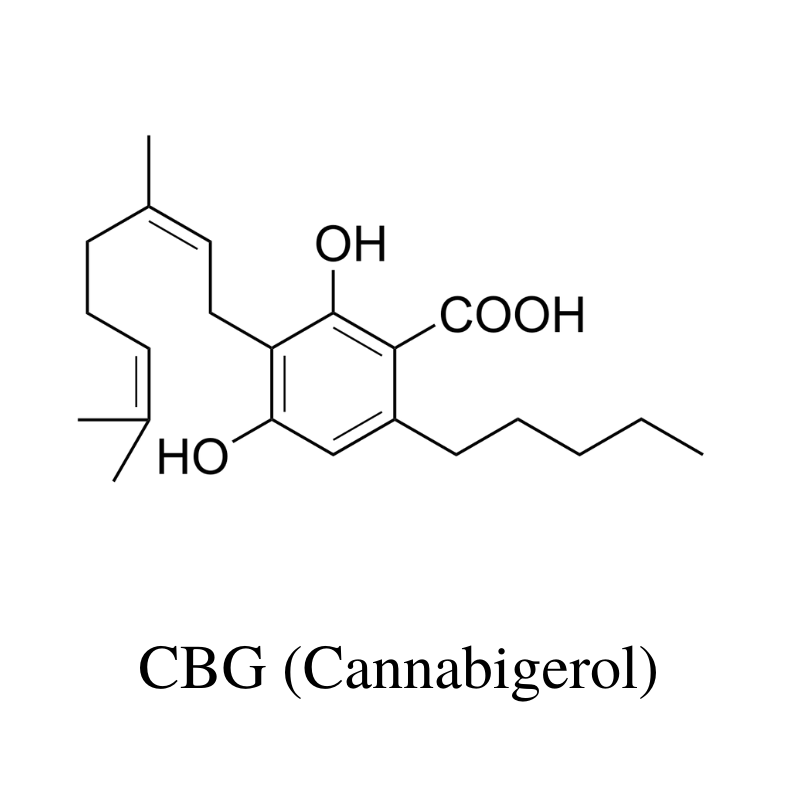
THC and CBD start as CBG — until things like time, temperature, and sunlight have their way with it.
It’s similar to CBD, but it’s actually energizing instead of calming. Oh, and good luck finding it. There are a few places that sell it, but it’s nowhere near as popular as CBD — yet. Like anything else, be careful when buying it.
CBC (Cannabichromene)
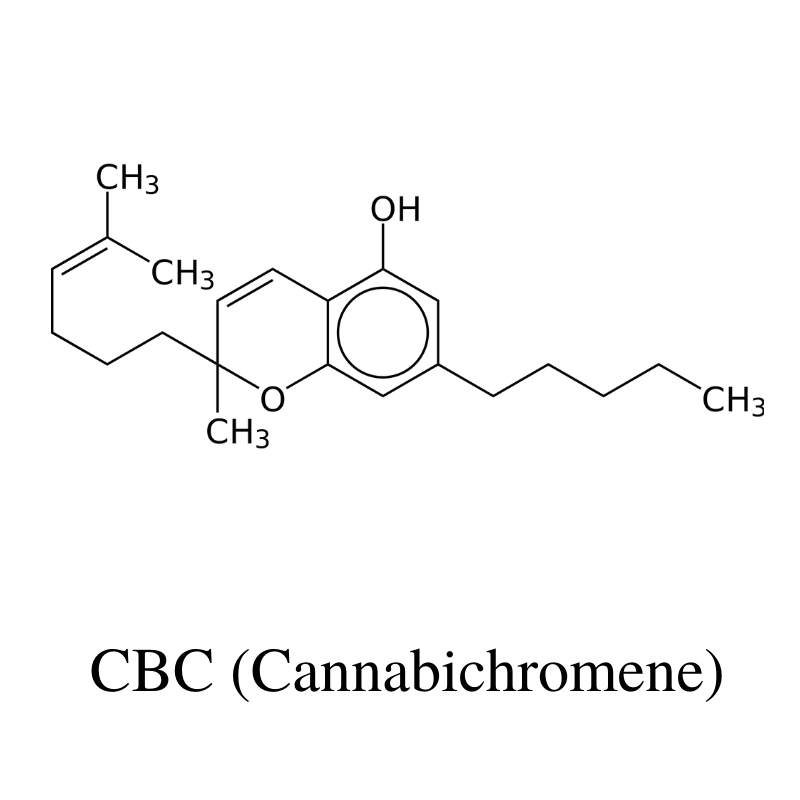
CBC can actually make up to more than half of the cannabinoid profile in Cannabis, but it’s not studied like THC or CBD. It pairs well with them, though, and might help improve acne, pain, and mood.
Other cannabinoids include:
- THCV (Tetrahydrocanabivarin)
- THCC (tetrahydrocannabiorcol)
- THCP (Tetrahydrocannabiphorol)
- THC-O (Tetrahydrocannabidiol-O-Acetate)
- HHC (Hexahydrocannabinol)
- CBDV (Cannabidivarin)
- CBGA (Cannabigerolic acid)
- THCA (Delta 9-tetrahydrocannabinolic acid)
- CBDA (Cannabidiolic acid)
- CBCA (Cannabichromenenic acid)
- CBGVA (Cannabigerovarinic acid)
- THCVA (Tetrahydrocanabivarinic acid)
- CBDVA (Cannabidivarinic acid)
- CBCVA (Cannabichromevarinic acid)
- Delta 8 THC
- Delta 10 THC
What’s the Connection Between TRP & Cannabinoids?
Know you know what TRP channels and cannabinoids are, but how do they affect each other?
While researchers studied TRPs for possible treatments, they discovered that cannabinoids could modulate TRP channels [19].
So far, six channels from three subfamilies (TRPV1-4, TRPA1, and TRPM8) seem to be affected by cannabinoid activity. Some researchers even call these channels “ionotropic cannabinoid receptors.”
Cannabinoid & TRP Research
As with everything else concerning the ECS, research is too limited to know the actual implications of this information. Still, it’s promising.
1. Studies on Delta 9 Tetrahydrocannabinol (THC) & TRP Channels
THC modulates TRPV2 the most, but it also affects TRPV3 and 4, TRPA1, and TRPM8. It doesn’t seem to act on TRPV1 at all.
2. Studies on Cannabidiol (CBD) & TRP Channels
CBD’s interaction with CB1 and CB2 remains somewhat of a mystery, though there are theories. We do know it has a strong affinity for TRPV1 and TRPM8 channels but also modulates many others.
3. Studies on Tetrahydrocannabivarin (THCV) & TRP Channels
THCV gets around kind of like CBD. Both have a reputation for being potent modulators of many TRP channels, especially TRPV1. Scientists call them “promiscuous” if that gives you a better description [19].
4. Studies on Cannabigerol (CBG) & TRP Channels
CBG interacts with sub-types of the TRPV channels and activates α2-adrenoreceptors [20].
Selective α2-adrenoceptor agonists are used to treat many disorders and have vast therapeutic potential.
5. Study on Cannabinoids, TRPs, & Possible Treatments
One study in 2010 looked at the impact cannabinoids have on various TRP channels to determine possible future treatments [21].
Here’s what the researchers found:
- CBD, CBG, CBGV, and THCV stimulated and desensitized human TRPV1.
- CBC, CBD, and CBN were potent TRPA1 agonists and desensitizers.
- THCV-BDS was the most potent TRPA1 agonist.
- CBG-BDS and THCV-BDS were the most potent rat TRPM8 antagonists.
- All non-acid cannabinoids, except CBC and CBN, potently activated and desensitized TRPV2.
This information implies that cannabinoids show great possibilities — beyond what we thought.
6. Studies on Other Connections Between TRPs & Cannabinoids
The more researchers study them, the more interconnected cannabinoids and TRP channels seem to be.
Endocannabinoids (anandamide or AEA and 2-arachidonoyl glycerol or 2-AG) help regulate synaptic transmissions, but the connection between the ECS and TRPs goes beyond that. In fact, TRPs are lovingly referred to as “ionotropic cannabinoids receptors” because of the role they play.
- An endogenous ligand of TRPV1 channels (specifically N-arachidonoyl-dopamine, in case you’re curious) acts like a cannabinoid.
- The endocannabinoid anandamide (AEA) is chemically similar to capsaicin, a xenobiotic ligand of TRPV1.
- There’s an overlap between the ligand recognition properties of some TRP channels and ECS proteins — CB1, CB2, and AEA cellular re-uptake catalysts.
The evidence keeps piling up, further proving that several TRP subtypes are a huge part of the ECS, making them a target for pain relief and for future medications with multiple mechanisms of action [22, 23].

Conclusion: Are TRPs & Cannabinoids the Future?
We know so little about the endocannabinoid system and how it works, but its connection with TRP channels seems promising. It only makes sense since the ECS and TRP channels play an obvious role in pain and other aspects of our health.
With more research, maybe we can tap into this magical duo and make tremendous progress in medicine.
References
- Song, M. Y., & Yuan, J. X. J. (2010). Introduction to TRP channels: structure, function, and regulation. Membrane Receptors, Channels, and Transporters in Pulmonary Circulation, 99-108.
- Numata, T., Kiyonaka, S., Kato, K., Takahashi, N., & Mori, Y. (2011). Activation of TRP channels in mammalian systems. TRP channels.
- Smani, T., Shapovalov, G., Skryma, R., Prevarskaya, N., & Rosado, J. A. (2015). Functional and physiopathological implications of TRP channels. Biochimica et Biophysica Acta (BBA)-Molecular Cell Research, 1853(8), 1772-1782.
- Jordt, S. E., & Ehrlich, B. E. (2007). TRP channels in disease. Calcium Signalling and Disease, 253-271.
- Messeguer, A., Planells-Cases, R., & Ferrer-Montiel, A. (2006). Physiology and pharmacology of the vanilloid receptor. Current neuropharmacology, 4(1), 1-15.
- Asghar, M. Y., & Törnquist, K. (2020). Transient receptor potential canonical (TRPC) channels as modulators of migration and invasion. International journal of molecular sciences, 21(5), 1739.
- Jimenez, I., Prado, Y., Marchant, F., Otero, C., Eltit, F., Cabello-Verrugio, C., … & Simon, F. (2020). TRPM Channels in Human Diseases. Cells, 9(12), 2604.
- Harteneck, C. (2005). Function and pharmacology of TRPM cation channels. Naunyn-Schmiedeberg’s archives of pharmacology, 371(4), 307-314.
- Thies, J., Neutzler, V., O’leary, F., & Liu, H. (2016). Differential Effects of TRPA and TRPV Channels on Behaviors of Caenorhabditis elegans. Journal of experimental neuroscience, 10, JEN-S32837.
- Venkatachalam, K., & Montell, C. (2007). TRP channels. Annu. Rev. Biochem., 76, 387-417.
- Samanta, A., Hughes, T. E., & Moiseenkova-Bell, V. Y. (2018). Transient receptor potential (TRP) channels. Membrane Protein Complexes: Structure and Function, 141-165.
- LopezJimenez, N. D., Cavenagh, M. M., Sainz, E., Cruz‐Ithier, M. A., Battey, J. F., & Sullivan, S. L. (2006). Two members of the TRPP family of ion channels, Pkd1l3 and Pkd2l1, are co‐expressed in a subset of taste receptor cells. Journal of neurochemistry, 98(1), 68-77.
- Wang, W., Zhang, X., Gao, Q., & Xu, H. (2014). TRPML1: an ion channel in the lysosome. Mammalian Transient Receptor Potential (TRP) Cation Channels, 631-645.
- Yue, L., & Xu, H. (2021). TRP channels in health and disease at a glance. Journal of Cell Science, 134(13), jcs258372.
- Lafaye, G., Karila, L., Blecha, L., & Benyamina, A. (2017). Cannabis, cannabinoids, and health. Dialogues in clinical neuroscience, 19(3), 309.
- Schrot, R. J., & Hubbard, J. R. (2016). Cannabinoids: medical implications. Annals of medicine, 48(3), 128-141.
- Baron, E. P. (2018). Medicinal properties of cannabinoids, terpenes, and flavonoids in Cannabis, and benefits in migraine, headache, and pain: an update on current evidence and cannabis science. Headache: The Journal of Head and Face Pain, 58(7), 1139-1186.
- Wise, J. (2018). FDA approves its first Cannabis based medicine.
- Muller, C., Morales, P., & Reggio, P. H. (2019). Cannabinoid ligands targeting TRP channels. Frontiers in molecular neuroscience, 11, 487.
- Kogan, N. M., Lavi, Y., Topping, L. M., Williams, R., McCann, F. E., Yekhtin, Z., … & Mechoulam, R. (2021). Novel CBG derivatives can reduce inflammation, pain and obesity. Molecules, 26(18), 5601.
- De Petrocellis, L., Ligresti, A., Moriello, A. S., Allarà, M., Bisogno, T., Petrosino, S., … & Di Marzo, V. (2011). Effects of cannabinoids and cannabinoid‐enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. British journal of pharmacology, 163(7), 1479-1494.
- Marzo, V. D., & Petrocellis, L. D. (2010). Endocannabinoids as regulators of transient receptor potential (TRP) channels: a further opportunity to develop new endocannabinoid-based therapeutic drugs. Current medicinal chemistry, 17(14), 1430-1449.
- Storozhuk, M. V., & Zholos, A. V. (2018). TRP channels as novel targets for endogenous ligands: focus on endocannabinoids and nociceptive signalling. Current neuropharmacology, 16(2), 137-150.