| Total CBD: | 500 – 2500 mg |
| Potency: | 16.6 - 83.3 mg/mL |
| Cost per mg CBD: | $0.12 – $0.18 |
| Extract Type: | Full-spectrum |
| THC Content: | <0.3% |

Evidence based
CBD Oil for Schizophrenia & Psychosis: Can It Help?
Schizophrenia is a neurological disorder affecting the perception of reality.
We explore if CBD is safe & how it might help.
Schizophrenia causes disordered thoughts and speech, visual or auditory hallucinations, and a myriad of other symptoms that can vary from one person to the next.
Researchers are continuously looking for new, effective treatment options for schizophrenia, and in recent years have turned their focus toward CBD — a powerful, medicinal (non-psychoactive) compound contained in the cannabis plant.
In this article, we’ll discuss what we know so far about this debilitating mental health condition and how CBD can be used to support symptoms.
Can CBD Help With Schizophrenia?
Schizophrenia is a complex psychiatric disorder involving many different confounding factors working together to produce symptoms. Schizophrenia is a serious chronic, debilitating psychotic disorder listed in the top 15 leading causes of disability worldwide according to the National Institute of Mental Health.
This means that there is no single effective treatment for the disorder. Successful treatment, therefore, requires an all-encompassing approach. Everything from changes in diet and lifestyle to supplements and medications should be combined to manage the condition.
CBD has been shown to offer some unique benefits that may be combined with other treatments to maximize the management of schizophrenia.
While the mechanism of action for CBD remains unclear, the results so far have been promising.
The potential benefits of CBD oil for schizophrenia include:
- Alleviates anxiety & depression
- Regulates neurotransmitter balance (dopamine, serotonin, & glutamate)
- Increased blood flow to cortical regions of the brain
- Improves sleep quality & duration
- Regulates the vanilloid receptors (TRPV1)

What is Schizophrenia?
Schizophrenia is a diagnosable psychotic disorder involving delusions, hallucinations, disorganized speech, difficulty staying focused, lack of motivation, and disorganized or catatonic behavior. Diagnosis by a physician requires at least a month or two or more symptoms over at least six months, with at least one positive symptom and social/occupational dysfunction.
Seeing a doctor early is important because schizophrenia must be carefully distinguished from other mood and psychotic disorders with similar symptoms, in order to optimize correct treatment and minimize long-term harm.
However, it’s a rare condition affecting ~1% of the US population, according to the American Psychiatric Association. They also note that approximately half of schizophrenia patients may also suffer from another mental or behavioral disorder.
There are a lot of misconceptions in public understanding of this condition. Despite popular belief, most schizophrenics aren’t dangerous. They don’t all live in hospitals nor have split personalities. Many, albeit not most people, who have the condition can live reasonably normal lives — they often have jobs and families and can live independently.
Schizophrenia affects both men and women equally, but symptoms tend to appear sooner in males than females. Men usually begin experiencing symptoms around their late-teens to mid 20s, while females typically start showing signs in their mid 20s or early 30s. It’s rarer for anybody under the age of 12, or over 40, to show symptoms of schizophrenia — but still possible.
Schizophrenia itself isn’t deadly, but it’s often associated with other medical conditions that can lead to problems later in life — such as heart disease or diabetes. Patients, in general, are at higher risk of premature death from such preventable causes, also including metabolic and liver disease, and suicide.
Three Phases of Schizophrenia
1. Prodromal Phase
This is the phase leading up to the first display of active psychotic symptoms, usually starting here with negative symptoms. “Negative” symptoms can be thought of as irregular social behaviors or speech/affect opposite of the norm (listed below). There is also some accompanying decline in daily functioning. If detected early enough, the onset and severity of schizophrenia can be significantly reduced and better managed in the long-term .
In the prodromal phase, patients often experience a decline in social and cognitive functions like memory, judgement, attention, depression, anxiety, isolation, and learning difficulties. Patients may also have mood symptoms such as depression, anxiety, and suicidal thoughts which should be taken seriously.
The prodromal phase can last anywhere from several weeks to several years [1].
2. Active Phase
During this phase, distinct positive symptoms become evident and perhaps more severe, involving delusions, hallucinations, and catatonic behavior. These “positive” symptoms may involve delusions, hallucinations, disorders of thought, and either agitation/aggression or catatonic behavior. This is when treatment is most important and when most schizophrenia diagnoses are made.
3. Residual Phase
In the residual phase, symptoms may begin to disappear, but patients are often left feeling “flat,” with poor motivation, low mood, and inability to focus or concentrate. Treatment during this phase is still important, directed toward controlling psychotic episodes and mood symptoms.
In the long run, about 30% will improve or return to normal function, another 30% will be hospitalized intermittently, and another 30% will be institutionalized or incapacitated. Unfortunately, ~10% of patients are lost to suicide.
Signs & Symptoms of Schizophrenia
The symptoms of schizophrenia can be divided into three main categories:
A) Positive (Psychotic) Symptoms
- Delusions
- Hallucinations
- Disorganized speech
- Disorganized behavior
- Catatonic behavior
- Psychosis
B) Negative Symptoms
- Changes in emotions
- Flat affect
- Apathy
- Less emotional expression
- Lack of energy (Anergia)
- Asociality
- Lack of detail in speech (Alogia)
- Loss of motivation (Avolition)
C) Cognitive Symptoms
- Poor memory
- Impaired judgement
- Learning difficulties
- Poor concentration
What Causes of Schizophrenia?
Unfortunately, there isn’t a single identified cause of schizophrenia. Research has linked the disorder with some different potential causes, including environmental influences, genetics (i.e. chromosome 6), changes in brain chemistry, and physical or emotional trauma.
1. Dopamine Theory
One of the leading theories for the causes of schizophrenia comes from early behavioral studies that found if you increase dopaminergic activity in certain brain pathways then psychotic symptoms appear (as in overdoses of cocaine, amphetamine, L-dopa).
This mesocorticolimbic projection is now the primary target mechanism of antipsychotic drugs.
In fact, all anti-psychotic medications work by blocking dopamine (D2) receptors in the brain to some degree — suggesting that schizophrenia is caused by too much dopamine in certain brain pathways.
The trade-off is that either over-activating or blocking dopamine in certain brain areas may cause unpleasant side-effects, which can be addressed.
For example, blocking dopamine receptors in one area produces Parkinsonian-like effects and involuntary muscle spasms. Too little dopamine activity in the frontal cortex is thought to cause the negative and cognitive symptoms.
First generation anti-psychotics are effective at blocking psychotic symptoms, however, they often come with many other side effects. Second generation (or “atypical”) anti-psychotics are better at avoiding the side-effect pathways, and also block a greater number of serotonin receptors.
2. Brain Structure Abnormality Theory
Neuroimaging studies have shown that patients with differing symptoms have physiological abnormalities (such as reduced blood flow) in different areas of the brain.
For example, patientshave been shown to have abnormalities in the thalamus — the area of the brain tasked with filtering and processing sensory signals such as sight, sound, or touch. Other studies have found that patients show signs of reduced neurons, which may be related to the faulty, overactive C4 pruning gene researchers found on chromosome 6.
All of these different factors suggest that schizophrenia can be caused by dysfunctions in many different areas of the brain. Symptoms will be determined by the parts of the brain that are most affected.
Low doses of cannabis improve blood flow to regions of the brain involved with regulating mood, sociability, and cognition — potentially reducing psychotic symptoms associated with schizophrenia [10].
3. Glutamate Theory
Glutamate is the most abundant neurotransmitter in the brain, and the one responsible for neural excitement. One theory regarding schizophrenia involves inappropriate glutamate activity and NMDA receptor expression alteration in the brain. This theory could be used to explain many of the symptoms associated with the condition. Additionally, the psychoactive drug phencyclidine (PCP) is known for producing acute, schizophrenia-like psychosis through activation of the glutamate receptors in the brain [8].
This has led some medical researchers to suggest schizophrenia involves similar over- or underactivation of glutamate in certain areas of the brain.
Studies show that synthetic cannabinoids reduce PCP-induced schizophrenic symptoms in rats [9].
4. Anandamide Excess Theory
Other research findings suggest schizophrenic patients have significantly higher levels of anandamide in their blood [4]. Follow up studies show high levels of anandamide present in the cerebrospinal fluid of actively psychotic, schizophrenic patients who have never been treated. Interestingly, researchers now pose that high anandamide may not be the cause, but is actually a homeostatic compensation to fight the disease state.
In a double-blind, randomized clinical trial, CBD was shown to improve psychotic symptoms by improving anandamide signalling. CBD was just as effective as the potent, second generation antipsychotic amisulpride at reducing symptoms — but had less unpleasant side effects.
CBD inhibits the enzyme FAAH from degrading anandamide, suggesting the endocannabinoid system is somehow altered in schizophrenia, but may now play a new role in treatment.
Similar studies report dysfunctional CB1 receptor activity in schizophrenic patients, especially in regions of the brain relating to cognition and memory — two functions highly compromised in schizophrenia [5, 6].
Patients with schizophrenia are more likely to be negatively affected by THC — which is a well-known CB1 receptor agonist [7].
This, of course, makes schizophrenia challenging to treat because there are so many different factors to take into account. It also explains why some patients respond to treatment, and others don’t.
5. Other Potential Causes
- Severe or long-term stress
- Substance abuse, particularly in adolescence
- Genetic factors
- Viral infection
- Developmental problems
- Autoimmune disorders
- Neurodegenerative disorders
Treatment Options for Schizophrenia
The most effective treatments for schizophrenia have an all-encompassing approach. Medications, lifestyle coaching, psychiatric care, and group therapy are all necessary aspects of treatment for this condition.

With early and proper treatment involving antipsychotic medications, most of the symptoms of schizophrenia can be reduced or eliminated, and episodes of active-phase schizophrenia become less frequent.
Unfortunately, all of these medications come with potentially negative side-effects, especially in the long term. Sudden, abnormal or painful muscle movements, diabetes, and heart complications are especially common in people taking these medications. There’s also a risk of CBD interacting with medications, so always talk to your doctor first.
However, side effects can be addressed with your doctor and managed if they appear. Families should seek support for their affected loved ones and themselves, with assistance like home care and ensuring patients can access and maintain treatment long-term.
Communities should provide opportunities for employment and assisted/independent living, giving patients a base from which to set and achieve goals.
Treatment for Schizophrenia May Include:
- Lifestyle coaching
- Dietary changes
- Addiction treatment
- Antipsychotic medications
- Psychiatric therapy
- Group therapy
Medications Often Used For Schizophrenia:
- Clozapine (Clozaril)
- Olanzapine (Zyprexa)
- Ziprasidone (Geodon)
- Aripiprazole (Abilify)
- Risperidone (Risperdal)
- Quetiapine (Seroquel)
- Haloperidol (Haldol)
What the Research Says: CBD Oil for Schizophrenia
Over the past decade, there’s been a growing interest in the use of CBD for treating schizophrenia.
This research started following a case report released in 1995 highlighting the improvement in a schizophrenic patient who was unresponsive to the standard antipsychotic medication haloperidol [3]. In 2012, the results of the clinical study highlighted above on CBD vs amulisopride and enhanced anandamide signalling was published.
Even more recently, the pharmaceutical company GW Pharmaceuticals Plc recently ran a series of clinical trials on a new CBD-based drug it’s been developing called Sativex®. One of these studies explored whether or not CBD was able to relieve symptoms of schizophrenia in patients who were unresponsive to standard antipsychotic medications [2].
The GW Pharmaceuticals study was a phase 2, double-blind clinical trial conducted across 15 different hospitals in the UK, Romania, and Poland. Patients in the study were randomly put into either a treatment group (using 1000 mg per day of CBD split into two doses) or a control group (using a placebo).
At the end of the six-week trial, the CBD group showed modest improvements in schizophrenic symptoms. The most substantial improvements from the study involved motor speed and executive functioning.
The most significant finding in this research was that CBD didn’t appear to rely on dopamine receptor modulation — which is the primary target for current schizophrenia treatments. Instead, researchers in this study suggested the mechanism of action to be through inhibition of fatty acid amide hydrolase (FAAH), inhibition of adenosine reuptake, vanilloid receptor activation (VR1), and serotonin (5HT1A) receptor activation [2].
They concluded by stating that: “Because CBD acts in a way different from conventional antipsychotic medication, it may represent a new class of treatment for schizophrenia.”
More clinical trials are scheduled to explore the use of CBD for schizophrenia in larger populations and longer duration of treatment.
Results of the GW Pharmaceuticals Research Study:
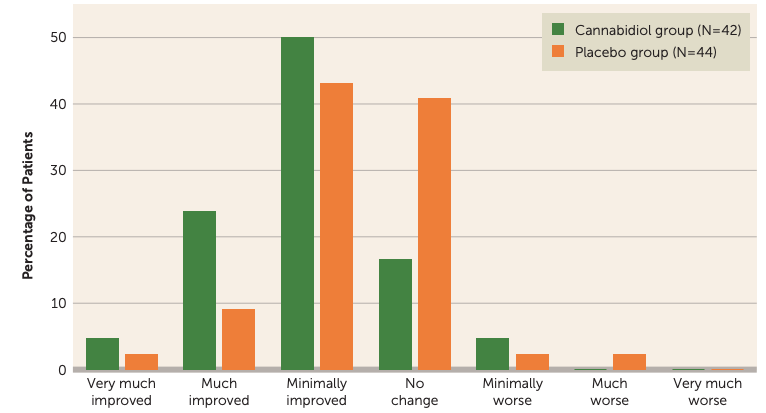
(Source: McGuire et al., 2017)
THC vs. CBD for Schizophrenia
High-THC and low-CBD extracts have been associated with a higher risk of psychotic episodes [11]. Other studies have shown that cannabis containing a high level of CBD and a level of low THC is associated with a lower risk of psychotic episodes [12].

Other studies have shown that CBD offered improvement in symptoms of schizophrenia to a similar degree as amisulpride — an antipsychotic medication [13]. CBD also had fewer side-effects.
The differences between CBD and THC and their effect on schizophrenia is very important — and likely to be the reason behind the conflicting evidence for cannabis users and schizophrenia. Some patients find relief from symptoms with cannabis use; others experience dramatically worsened symptoms after using cannabis.
It is not recommended, but if using cannabis for schizophrenia, make sure you pay attention to the THC content. Additionally, only choose products with low or “not detectable” THC concentrations when buying CBD.
Key Takeaways: Using CBD for Schizophrenia
Schizophrenia is a highly complex neurological disorder that continues to puzzle medical researchers. However, there are several significant theories about the underlying causes of schizophrenia.
Some patients respond very well to medications; others do not.
Although CBD may improve the side-effects of the condition using several different models of schizophrenia (clinical and PCP-induced), there is also evidence that other cannabinoids — namely THC — can worsen schizophrenia.
For this reason, it’s recommended that you only use CBD for schizophrenia under the close watch of a medical professional. It’s also recommended that you only use CBD products that are entirely void of THC. Additionally, research suggests that a high dose (1000 mg per day) of CBD is needed to produce even modest improvements in symptoms.
Patients and families are encouraged to seek further support and resources from their doctor, and groups like NAMI and the American Psychiatric Association.
Tips For Getting the Most From CBD Oil For Schizophrenia
- Remember there is no cure for schizophrenia — including CBD. Currently approved treatments are designed to manage the condition, not cure it.
- Avoid any cannabis extracts with more than 0.3% THC — this can have a negative impact on schizophrenia over time. Stick to CBD isolates or other THC-free extracts.
- Use only high-quality, third-party-tested CBD products to avoid contaminated products that can worsen symptoms.
- Always discuss CBD or other supplement use with your doctor before taking it — some medications may have negative side-effects if mixed with CBD or other cannabinoids.
References Cited In This Article
- Larson, M. K., Walker, E. F., & Compton, M. T. (2010). Early signs, diagnosis, and therapeutics of the prodromal phase of schizophrenia and related psychotic disorders. Expert review of neurotherapeutics, 10(8), 1347-1359.
- McGuire, P., Robson, P., Cubala, W. J., Vasile, D., Morrison, P. D., Barron, R., … & Wright, S. (2017). Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. American Journal of Psychiatry, 175(3), 225-231.
- Zuardi, A. W., Morais, S. L., Guimaraes, F. S., & Mechoulam, R. (1995). Antipsychotic effect of cannabidiol. The Journal of clinical psychiatry.
- De Marchi, N., De Petrocellis, L., Orlando, P., Daniele, F., Fezza, F., & Di Marzo, V. (2003). Endocannabinoid signalling in the blood of patients with schizophrenia. Lipids in health and disease, 2(1), 5.
- Eggan, S. M., Hashimoto, T., & Lewis, D. A. (2008). Reduced cortical cannabinoid 1 receptor messenger RNA and protein expression in schizophrenia. Archives of general psychiatry, 65(7), 772-784.
- Zavitsanou, K., Garrick, T., & Huang, X. F. (2004). Selective antagonist [3H] SR141716A binding to cannabinoid CB1 receptors is increased in the anterior cingulate cortex in schizophrenia. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 28(2), 355-360.
- Pertwee, R. G. (2008). The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: Δ9‐tetrahydrocannabinol, cannabidiol and Δ9‐tetrahydrocannabivarin. British journal of pharmacology, 153(2), 199-215.
- Javitt, D. C., & Zukin, S. R. (1991). Recent advances in the phencyclidine model of schizophrenia. The American journal of psychiatry, 148(10), 1301.
- Spano, M. S., Fadda, P., Frau, R., Fattore, L., & Fratta, W. (2010). Cannabinoid self-administration attenuates PCP-induced schizophrenia-like symptoms in adult rats. European Neuropsychopharmacology, 20(1), 25-36.
- Cohen, M., Solowij, N., & Carr, V. (2008). Cannabis, cannabinoids and schizophrenia: integration of the evidence. Australian & New Zealand Journal of Psychiatry, 42(5), 357-368.
- Di Forti, M., Morgan, C., Dazzan, P., Pariante, C., Mondelli, V., Marques, T. R., … & Butt, A. (2009). High-potency cannabis and the risk of psychosis. The British Journal of Psychiatry, 195(6), 488-491.
- Schubart, C. D., Sommer, I. E., van Gastel, W. A., Goetgebuer, R. L., Kahn, R. S., & Boks, M. P. (2011). Cannabis with high cannabidiol content is associated with fewer psychotic experiences. Schizophrenia research, 130(1-3), 216-221.
- Deiana, S. (2013). Medical use of cannabis. Cannabidiol: a new light for schizophrenia?. Drug testing and analysis, 5(1), 46-51.
- Jochen Kindler, Frauke Schultze-Lutter, Martinus Hauf, Thomas Dierks, Andrea Federspiel, Sebastian Walther, Benno G Schimmelmann, Daniela Hubl, Increased Striatal and Reduced Prefrontal Cerebral Blood Flow in Clinical High Risk for Psychosis, Schizophrenia Bulletin, Volume 44, Issue 1, January 2018, Pages 182–192,
More Health Benefits to Explore
-
Conditions Related to Health Benefits
- CBD For Allergies: Can This Cannabinoid Ease Symptoms?
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- CBD For Psoriasis: Can CBD Help to Alleviate Symptoms?
- Traumatic Brain Injury (TBI)
- Arthritis
- Anxiety & Depression
- Weight Loss
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Antibiotic Resistance
- Asthma
- Atherosclerosis
- Autism
- Acne
- Bipolar Disorder
- Pain
- Crohn's Disease & Ulcerative Colitis
- Diabetes
- Epilepsy
- Endocrine Disorders
- Fibromyalgia
- Fatty Liver Disease
- Glaucoma
- Hypertension
- Heart Disease
- Huntington's Disease
- Inflammation
- Irritable Bowel Syndrome (IBS)
- Kidney Disease
- Migraine Headaches
- Muscle Recovery
- Multiple Sclerosis
- Motion Sickness
- Metabolic Syndrome
- Neurodegeneration
- Cancer
- Nausea
- Neuropathic (Nerve) Pain
- Osteoporosis/Bone Health
- Obsessive-Compulsive Disorder (OCD)
- Polycystic Ovarian Syndrome (PCOS)
- PTSD
- Prion/Mad Cow Disease
- Premenstrual Syndrome (PMS)
- Parkinson’s Disease
- Schizophrenia
- Sickle Cell Anemia
- Stroke
-
Conditions Related to Products
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 10 CBD Oils For Back Pain
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Terpene Concentrates
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- Best Dry Herb Vaporizers
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
Conditions Related to Topicals
-
Conditions Related to Oils & Tinctures
-
Conditions Related to Edibles
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Honey
- CBD Chewing Gum
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Coffee
- CBD Drinks & Shots
- CBD Capsules
-
Conditions Related to Gummies
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
-
Conditions Related to Hemp Flower
-
-
Conditions Related to Terpenes
-
-
Conditions Related to Cultivation
-
Conditions Related to Concentrates
-
Conditions Related to Delta 8 THC
-
Conditions Related to Delta 9 THC
-
-
-
-
Conditions Related to CBD
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
-
Conditions Related to THC-O
-
-
Conditions Related to Joint Health
-
Conditions Related to Pain Disorders
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Traumatic Brain Injury (TBI)
- Arthritis
- Pain
- Fibromyalgia
- Glaucoma
- Inflammation
- Kidney Disease
- Migraine Headaches
- Multiple Sclerosis
- Neuropathic (Nerve) Pain
- Premenstrual Syndrome (PMS)
- Sickle Cell Anemia
-
Conditions Related to Autoimmune Disease
-
Conditions Related to Cognitive Health
-
Conditions Related to Metabolic Disorders
-
Conditions Related to Psychological Disorders
-
Conditions Related to Muscles & Bones
-
Conditions Related to Nervous System
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- Traumatic Brain Injury (TBI)
- Anxiety & Depression
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Autism
- Bipolar Disorder
- Epilepsy
- Huntington's Disease
- Inflammation
- Migraine Headaches
- Multiple Sclerosis
- Motion Sickness
- Neurodegeneration
- Neuropathic (Nerve) Pain
- Obsessive-Compulsive Disorder (OCD)
- PTSD
- Prion/Mad Cow Disease
- Parkinson’s Disease
- Schizophrenia
-
-
Conditions Related to Reproductive Health
-
Conditions Related to Hormones & Endocrine
-
Conditions Related to Skin Health
-
Conditions Related to Cardiovascular System
-
Conditions Related to Digestive System
-
Conditions Related to Genetic Disorders
-
Conditions Related to For Children