| Total CBD: | 500 – 2500 mg |
| Potency: | 16.6 - 83.3 mg/mL |
| Cost per mg CBD: | $0.12 – $0.18 |
| Extract Type: | Full-spectrum |
| THC Content: | <0.3% |

Evidence based
Antibiotic Resistance and CBD: Current Research & Understanding
Antibiotic resistance is a serious problem in the modern world. CBD may be able to help by blocking the ability for bacteria to withstand their effects.
Antibiotic resistance is a major threat to public health.
The common drug-resistant bacteria MRSA (methicillin-resistant Staphylococcus aureus) is responsible for more deaths per year than HIV [1].
Every year, more and more strains of infectious bacteria become resistant to our medicine. On top of this, in the past 30 years, only 1 new class of antibiotic has been developed.
At these current rates, we won’t be able to defend ourselves against infectious disease for much longer.
Cannabis, as the wildcard it is, offers a unique solution to this problem.
Many of the cannabinoids in the plant prevent the ability of bacteria to resist the drugs we use to kill them.
Here, we discuss how cannabis is effective for preventing drug resistance and what the limitations are.
Summary: Using Cannabis for Preventing Drug-Resistance
We’ll get into the details of drug resistance and how CBD oil can be used to prevent it later on.
For now, let’s just gain some context as to how this works.
A number of studies on several cannabinoids have shown that they can interrupt a bacteria’s ability to resist antibiotic treatment.
Most of these studies are focused on a strain of drug-resistant bacteria that infects the skin, known as Methicillin-Resistant Staphylococcus aureus (MRSA).
Finding a high-quality CBD oil product containing the entire array of phytochemicals in the hemp plant is going to be the best option for drug-resistance. These oils are often referred to as “full-spectrum” extracts.
You can apply these oils directly to the skin along with your prescribed antibiotics.
Research is still being done to determine the potency of these oils when taken orally and the dosage needed for them to work.
CBD Oils For Antibiotic Resistance
The Dangers of Drug Resistance
Over the past 80 years, bacterial infection is relatively low on the list of concerns for doctors and patients alike.
This is because since the early 1930s we’ve had effective antibiotics for treating these infections.
Prior to this, bacterial infection was a common cause of death. In fact, people born before the 1930s had an average life expectancy of about 47 years [3].
Infectious diseases such as smallpox, cholera, diphtheria, pneumonia, typhoid fever, tuberculosis, and syphilis were both common and deadly.
We lacked effective treatments for these infections—a mere papercut could result in death to those who were unlucky enough to contract a dangerous bug.
The History of Antibiotics
Antibiotics changed everything.
In 1928, a Scottish microbiologist named Alexander Fleming accidentally discovered a mold species known as Penicillium notatum growing in a petri dish.
What was peculiar about this mold was that it was killing the bacteria around it.
Over the next decade, Fleming developed this into the medicine we now know as penicillin.
This forever changed the way we perform medicine.
Since the invention of penicillin, we no longer had to worry about bacterial infection. We had the treatment that could kill virtually any invading bacteria we contracted.

Antibiotic Resistance Started in the 1940s
Three years before antibiotics were even released to the public, the scientists developing them already started seeing signs of resistance. However, the real problem started when a strain of Staphylococcus became resistant to penicillin in 1940.
Subsequently, the following bacterias mutated: tetracycline-resistant Shigella in 1959, methicillin-resistant Staphylococcus in 1962, penicillin-resistant Pneumococcus in 1965, and erythromycin-resistant Staphylococcus in 1968.
Over the next 50 years, drug resistance skyrocketed. We now have resistant strains popping up every single year.
Modern Day Drug Resistance
A report published by the CDC in 2016 highlighted how serious this issue actually is.
At least 2 million people become infected with antibiotic-resistant bacteria each year and more than 23,000 people die annually as a consequence of these infections.
As more of these bugs become resistant to medication, this number is sure to rise substantially.
In the past couple of years, a new strain of the bacteria responsible for typhoid fever has emerged around Pakistan, showing resistance to all but one antibiotic.
As soon as it develops resistance to our last remaining option, there will be nothing available to treat it.
Examples of Common Drug-Resistant Bacteria Strains
- Penicillin-Resistant Streptococcus pneumonia (PRSP)
- Methicillin-Resistant Staphylococcus aureus (MRSA)
- Vancomycin-Resistant Enterococci (VRE)
- Multiple-Drug-Resistant Gram-Negative Bacilli (MDRGNB)
- Extensively Drug-Resistant Typhoid (XDR Typhoid)
- Extensively Drug-Resistant Tuberculosis (XDR Tuberculosis)
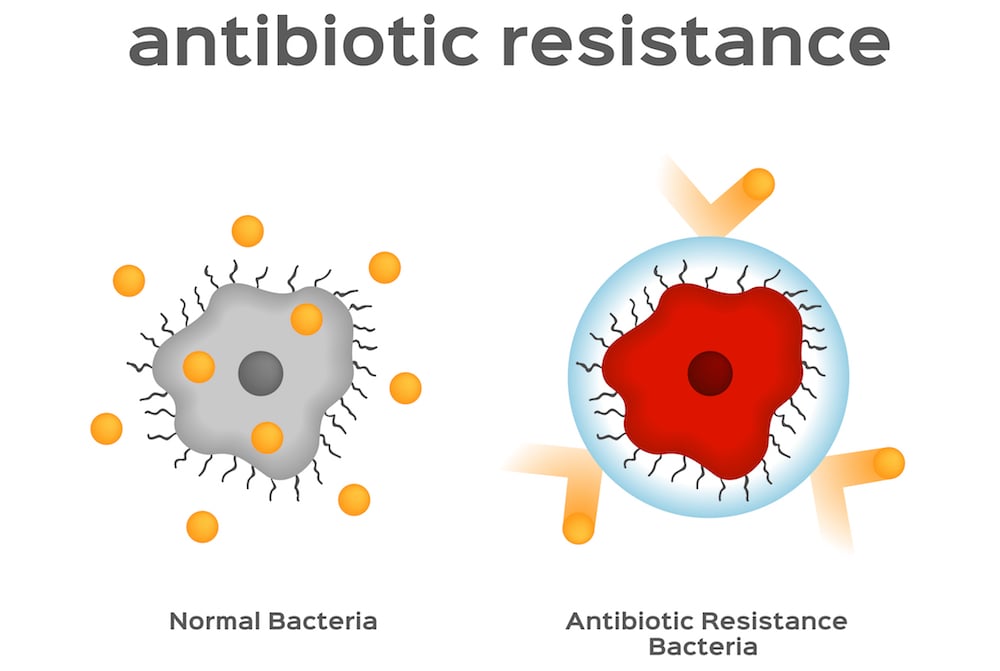
How Does Drug Resistance Work?
So how does drug resistance work? And how can CBD oil prevent it?
Let me explain with an overview of how antibiotics kill bacteria.
How Antibiotics Kill Bacteria
There are many different kinds of antibiotics, but the majority of them works in the same way:
Antibiotics prevent bacteria from growing.
If the bacteria can’t grow or multiply, they won’t have the potential for much damage.
Bacteria wreak havoc in numbers. A single bacteria, or even a few hundred, will have little effect on the body.
When we start to get a few hundred thousand or a few million, however, these organisms can cause serious damage.
Antibiotics work by blocking specific parts of the bacteria needed for growth.
For better understanding, let’s compare these mechanisms to a construction site. The construction site is the bacteria, working on building new bacteria to infect new areas of the body.
A few common examples of antibiotics include:
1. Beta-lactams
These block the bacteria’s ability to build their cell wall. When this happens, the cells begin to tear apart as they grow, causing the insides to leak out. This, of course, is fatal for the bacteria.
It’s like opening the gates to a construction site and letting all the workers leave, taking their tools with them. When nobody is left to do the work, the site is eventually abandoned.
2. Macrolides
Macrolides stop cell growth by attacking the RNA. This is the part of the cell responsible for building new proteins.
No proteins mean no growth. Since proteins are responsible for everything a bacteria does, it essentially disables them. They float around aimlessly before eventually dying.
This is like destroying the machinery on a job site. Nobody will be able to do any work, and the job will eventually be abandoned altogether.
3. Quinolones
Quinolones attack the DNA of bacteria directly.
DNA gives all directions and instructions on how the cell is supposed to work. If these are broken, the cell is unable to build anything and will quickly die as a result.
It’s like going into a construction site, completely destroying the blueprints and dismissing the master builder. The workers will try to keep going, but don’t know how to do their jobs effectively. The building will likely fall apart before it’s ever finished.
How Bacteria Become Resistant
The lifespan of bacteria is very short.
But even so, like all organisms on earth, they are subjected to natural selection and evolutionary changes. Eventually, this evolution will lead to bacteria that are adapted to resist antibiotics.
Let me explain.
Every time a bacteria is made, there is a small chance its DNA will suffer a mutation somewhere. Most of the time this change does nothing. It is neutral.
But occasionally, this mutation has an effect. It can make the bacteria either stronger or weaker.
How? Natural selection. The stronger bacteria have a better chance of surviving, passing on its strong genes into the next generation. Meanwhile, the weaker bacteria are in a disadvantage, dying out and taking its “weak” genes out of the genetic pool.
Through random trial and error, and over the course of many generations, these mutations will eventually make that bacteria population more successful at doing its job. A bacteria’s job, like all life on earth, is to stay alive long enough to reproduce.
How does this work for drug resistance?
Let’s say we have 100 bacterial cells. Each one is the same but has one subtle mutation in its genetic code.
We then soak these bacteria in antibiotics.
The vast majority of these bacteria will die off. However, by chance, one of them manages to survive. Its unique, random mutation protected it from the antibiotics. This lonely little bacteria will reproduce, making more identical copies of itself with the same mutation.
Eventually, this bacteria will build a colony of millions, all sharing the same genetic mutation allowing them to resist the antibiotics.
This is a simple example of how drug resistance occurs. The only difference is that, instead of 100 bacterial cells, there are trillions. And instead of 1 type of antibiotics, there are dozens.
Every time we use antibiotics – especially if we do it unnecessarily and too often – we favor the bacteria that are able to resist them. Over the years, the bacteria become tougher and harder to fight.
How Bacteria Stop Antibiotics from Working
The genetic mutations bacteria have developed that allow them to resist antibiotics can vary, but the most common method is to actually pump the antibiotic out of the bacteria once it gets inside.
This prevents the antibiotic from doing its job and killing the cell.
The specialized pumps on bacteria that do this are referred to as efflux pumps.
These efflux pumps were found in the membranes of many bacteria, but they were designed to remove other compounds from the cell-like toxic metabolic byproducts, and neurotransmitters.
With drug resistance, these pumps are adapted to pump out antibiotics as well.
This finally gets us to the point of this article…
How do Cannabinoids like CBD Prevent Drug Resistance?
Now that we understand how bacteria can become resistant to antibiotics, we can talk about how cannabinoids prevent it.
Cannabinoids have a wide variety of effects on the human body.
They regulate homeostasis through the endocannabinoid system, stimulate the serotonin receptors to produce the characteristic “high” and activate receptors in the body responsible for muting pain signals.
Cannabinoids also inhibit the efflux pumps on bacteria.
Being fat-soluble compounds, the cannabinoids are able to interact with the fatty membranes of bacterial cells, and possibly alter the way they work.
Research is currently underway to identify these effects in human trials and to better understand the specific mechanism that makes them so effective.
Which Cannabinoids are the Best for Resisting Antibiotic-Resistance?
One of the primary studies on these effects looked at the 5 most abundant cannabinoids in the plant: CBD, CBC, CBG, CBN, and THC.
All of these cannabinoids were shown to have the ability to block the efflux pumps in drug-resistant strains of Staphylococcus aureus (MRSA), however, the non-psychoactive cannabinoids CBD and CBG showed the strongest results[2].
Most of the research currently underway is focusing on MRSA skin infections.
These infections are extremely common in hospitals and are proving to be an emerging global threat.
Topical cannabis salves are tested to inhibit the growth of these bacteria and allow antibiotics to do their job.
Cosmetic companies are also looking at cannabinoids as a new preservative to add to their products to prolong shelf life and resist bacterial colonies from forming.
How to Find CBD Oil That Will Offer These Benefits
In the United States, CBD oil is completely legal as long as it doesn’t contain anything above 0.3% THC.
There are a few different options you’re faced with when shopping for any cannabis oil:
1. CBD Isolates
CBD isolates are an extraction of the cannabis plant that only includes CBD.
All the terpenes, fiber, plant sugars, and proteins are removed to leave a high-potency CBD extract.
Although this may be effective in treating antibiotic resistance, it’s unlikely that this will offer the same benefit as a product that contains the other phytochemicals, adding its own benefits to the prevention of antibiotic.
2. Full-Spectrum Hemp Oil
Full-spectrum hemp oil is the most recommended product for delivering antibiotic-resistant benefits.
This is because the 2 strongest cannabinoids are the non-psychoactive CBD and CBG, both of which are found in high concentrations in full-spectrum hemp.
In addition to these cannabinoids, the entire phytochemical makeup of the plant is also found in this extract. The terpenes, flavonoids, minerals, and plant sugars can contribute to its effect profile.
3. THC Oils
THC oils are only available in states that have legalized recreational marijuana. They are also available in countries such as Canada or the Netherlands, that have legal marijuana products for sale.
THC oils often contain a spectrum of cannabinoids, including CBD, CBG, CBC, CBN, and THC, but are referred to as THC oils because they produce psychoactive effects.
If these products are available, and you aren’t opposed to receiving the psychoactive effects of the plant, this may be the best option.

Using CBD Oil to Prevent Antibiotic Resistance
More research is needed to assess the proper dose of CBD oil and other cannabis oils for preventing antibiotic resistance in bacteria.
Most of the current research involves the topical use of the herb for treating skin infections of MRSA.
With that said, the best options are full-spectrum CBD oils, containing as much of the plant’s cannabinoid and terpene content as possible. It also requires high dosing along with a combination of other therapies for best results.
References
- Bancroft, E. A. (2007). Antimicrobial resistance: it’s not just for hospitals. Jama, 298(15), 1803-1804.
- Appendino, G., Gibbons, S., Giana, A., Pagani, A., Grassi, G., Stavri, M., … & Rahman, M. M. (2008). Antibacterial cannabinoids from Cannabis sativa: a structure-activity study. Journal of natural products, 71(8), 1427-1430.
- Adedeji, W. A. (2016). The treasure called antibiotics. Annals of Ibadan postgraduate medicine, 14(2), 56.
Conditions that May Respond to Cannabidiol
-
Conditions Related to Health Benefits
- CBD For Allergies: Can This Cannabinoid Ease Symptoms?
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- CBD For Psoriasis: Can CBD Help to Alleviate Symptoms?
- Traumatic Brain Injury (TBI)
- Arthritis
- Anxiety & Depression
- Weight Loss
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Antibiotic Resistance
- Asthma
- Atherosclerosis
- Autism
- Acne
- Bipolar Disorder
- Pain
- Crohn's Disease & Ulcerative Colitis
- Diabetes
- Epilepsy
- Endocrine Disorders
- Fibromyalgia
- Fatty Liver Disease
- Glaucoma
- Hypertension
- Heart Disease
- Huntington's Disease
- Inflammation
- Irritable Bowel Syndrome (IBS)
- Kidney Disease
- Migraine Headaches
- Muscle Recovery
- Multiple Sclerosis
- Motion Sickness
- Metabolic Syndrome
- Neurodegeneration
- Cancer
- Nausea
- Neuropathic (Nerve) Pain
- Osteoporosis/Bone Health
- Obsessive-Compulsive Disorder (OCD)
- Polycystic Ovarian Syndrome (PCOS)
- PTSD
- Prion/Mad Cow Disease
- Premenstrual Syndrome (PMS)
- Parkinson’s Disease
- Schizophrenia
- Sickle Cell Anemia
- Stroke
-
Conditions Related to Products
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 10 CBD Oils For Back Pain
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Terpene Concentrates
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- Best Dry Herb Vaporizers
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
Conditions Related to Topicals
-
Conditions Related to Oils & Tinctures
-
Conditions Related to Edibles
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Honey
- CBD Chewing Gum
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Coffee
- CBD Drinks & Shots
- CBD Capsules
-
Conditions Related to Gummies
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
-
Conditions Related to Hemp Flower
-
-
Conditions Related to Terpenes
-
-
Conditions Related to Cultivation
-
Conditions Related to Concentrates
-
Conditions Related to Delta 8 THC
-
Conditions Related to Delta 9 THC
-
-
-
-
Conditions Related to CBD
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
-
Conditions Related to THC-O
-
-
Conditions Related to Joint Health
-
Conditions Related to Pain Disorders
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Traumatic Brain Injury (TBI)
- Arthritis
- Pain
- Fibromyalgia
- Glaucoma
- Inflammation
- Kidney Disease
- Migraine Headaches
- Multiple Sclerosis
- Neuropathic (Nerve) Pain
- Premenstrual Syndrome (PMS)
- Sickle Cell Anemia
-
Conditions Related to Autoimmune Disease
-
Conditions Related to Cognitive Health
-
Conditions Related to Metabolic Disorders
-
Conditions Related to Psychological Disorders
-
Conditions Related to Muscles & Bones
-
Conditions Related to Nervous System
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- Traumatic Brain Injury (TBI)
- Anxiety & Depression
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Autism
- Bipolar Disorder
- Epilepsy
- Huntington's Disease
- Inflammation
- Migraine Headaches
- Multiple Sclerosis
- Motion Sickness
- Neurodegeneration
- Neuropathic (Nerve) Pain
- Obsessive-Compulsive Disorder (OCD)
- PTSD
- Prion/Mad Cow Disease
- Parkinson’s Disease
- Schizophrenia
-
-
Conditions Related to Reproductive Health
-
Conditions Related to Hormones & Endocrine
-
Conditions Related to Skin Health
-
Conditions Related to Cardiovascular System
-
Conditions Related to Digestive System
-
Conditions Related to Genetic Disorders
-
Conditions Related to For Children