Evidence based
New Study Finds CBDA & CBGA May Block Cellular Entry of SARS-CoV-2
New research suggests cannabis may prevent the entry of the virus that causes COVID-19.
But it doesn’t work if you smoke or vape it.
New research conducted by researchers at Oregon State University found that two cannabinoids may offer protection against the virus that causes COVID-19 [1].
Before you grab your bong to acquire some of this so-called “herb immunity,” it’s important to note that this protective action isn’t offered from smoking the plant. Only the raw, non-decarboxylated forms of these cannabinoids were found to have any effect.
Let’s dig into the details of this study. We’ll examine what researchers discovered, what makes it significant and highlight some of the study’s shortcomings.
Examining Study Findings: Can Cannabis Prevent COVID-19?
Richard van Breeman, a lead researcher at the Linus Pauling Institute at Oregon State University, and his team used a unique mass spectrometry-based assay test to screen a variety of cannabinoids for their effects against SARS-CoV-2.
The study found two cannabinoids in particular — CBDA and CBGA — had the capacity to bind themselves to the spike protein that’s responsible for gaining the virus entry into the cell.
By blocking the virus’ ability to infect the cell, CBDA and CBGA may be useful for shortening the course of COVID-19 and reducing both the severity and transmissibility of the virus.
Study Details
So how does this research work? How were researchers able to determine the effectiveness (or lack thereof) from cannabinoids?
This research was conducted in test tubes and in computer simulations. Researchers incubated live SARS-CoV-2 virus’ with 25 μg/mL of either CBDA, CBGA, or vehicle control (DMSO). The viruses were then used to infect Vero E6 cells (a type of cell often used for viruses that replicate slowly).
A stain was then used to detect the presence of viral RNA within the cells.
In simple terms: if the cells became stained, it means the virus was able to enter the cell (AKA infection). If the cells didn’t stain, it means the virus was prevented from penetrating into the cell.
The study found that cells treated with either CBDA or CBGA didn’t show any staining — demonstrating a lack of entry by SARS-CoV-2.
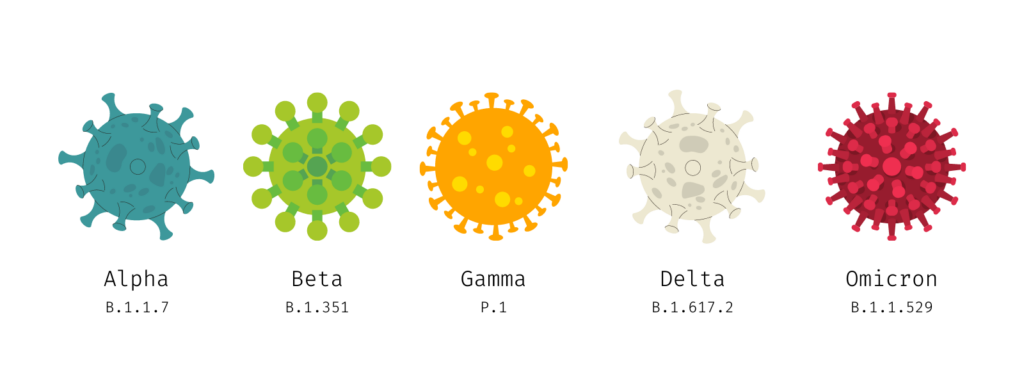
This study tested SARS-CoV-2 variants B.1.1.7 (alpha) and B.1.351 (beta), and both were effectively denied access after incubation with CBDA and CBGA.
Delta (B.1.617.2) and Omicron (B.1.1.529) variants have not yet been tested.
Only “Raw” Cannabinoids Were Found Effective Against SARS-CoV-2
While many people are jumping to the conclusion that they need to smoke more weed to reduce the chances of contracting COVID-19 because of this study — this isn’t accurate.
The study found that only the raw forms of CBD and CBG (CBDA and CBGA, respectively) had the capacity to bind to the SARS-CoV-2 spike protein and prevent entry into the cell.
So what are “raw” cannabinoids? What’s the difference between CBDA and CBD, or CBGA and CBG?
The main difference between the raw form and “activated” forms of cannabinoids is the presence of a carboxylic acid group in their molecular structure.
The cannabis plant only makes these cannabinoids in their acidic form. They need to be decarboxylated (heat-activated) in order to remove this carboxylic acid. This is usually done by smoking or vaping weed. The heat during these processes cleaves the carboxylic acid off the molecule, converting CBDA to CBD, CBGA to CBG, and THCA to THC.
Related: What is decarboxylation of cannabinoids? How does it work?
Caveats & Limitations Of This Study
While the findings in this study are impressive and will certainly be used to fuel further studies on the effects of CBDA and CBGA as a potential treatment or prevention for SARS-COV-2 infection, it’s important to keep things in context.
This study DOES NOT serve as sufficient proof that cannabinoids can prevent or even reduce the severity of COVID-19.
There were two main limitations with this study:
A) This Is In Vitro Research (Test Tube Studies)
The bottom line here is that this was an in vitro study — meaning that the tests were conducted in test tubes. The human system is significantly more complex, and in many cases, the results we see during in vitro studies don’t transfer to the human system.
For example, you could have a petri dish with cultured cancer cells sitting on a table. If you were to shoot the dish with a handgun, the cancer cells would surely die. From this research, you could deduce that handguns kill cancer. But this doesn’t mean anything when it comes to treating cancer in the human body.
The bottom line is that in vitro research is an important step, but we can’t draw any clinical conclusions from it until we know what happens in live systems — either through animal testing or clinical trials involving humans.
Since CBDA and CBGA have already been confirmed safe through numerous testing, it’s possible we’ll be able to skip Phase I trials while exploring this effect, saving a year or more of research.
B) The Effective Dose of Cannabinoids Used in the Study May Not Be Practical
The concentration of cannabinoids used in this study was extremely high (100 to 0.625 μg/mL). It’s unclear if it’s even possible to achieve these levels of cannabinoids in the human body — especially through oral consumption.
With that said, studies on dogs have shown that doses of 1 mg/kg CBDA (orally) had a high bioavailability and were well tolerated (produced little to no side effects) [2]. This is a very high dose. The average dose of CBD is around 25–50 mg, which works out to around 0.3 mg/kg.
It’s important to keep in mind that doses this high are going to be very expensive as well. The cost per milligram of CBDA is around $0.15 and CBGA closer to $0.22.
In the United States, the average man weighs 90 kg, and the average woman weighs 77 kg.
This means a single 1 mg/kg dose would cost between $13 and $20 for men and $11 and $17 for women.
Additionally, it’s very likely that in practice, we’d need to take 2, 3, or even 4 doses per day to maintain this protective effect. So in order to get the protective action of CBDA and CBGA, the cost per day could easily exceed $50 per day ($1500 per month) — which simply isn’t feasible for most people.
Tips For Finding & Using Raw Cannabinoids
Whenever you smoke or vape weed or take CBD products, you’re using the decarboxylated version of these cannabinoids.
This study clearly shows these decarboxylated forms don’t work against COVID-19. This means the carboxylic acid group on raw cannabinoids is necessary for deactivating the spike protein on the SARS-CoV-2 virus.
What this means is that instead of conventional CBD products, you’ll need to seek out specially-designed “raw” CBD oils that maintain high concentrations of CBDA or CBGA instead.
Raw cannabinoid products are more difficult to find than decarboxylated products for two reasons:
- Raw cannabinoids are sensitive to heat. Conventional extraction methods require heat for separating cannabinoids and solvents, so new methods must be adopted instead, which may have a lower efficiency than solvent-based extraction.
- There’s less demand for raw cannabinoids than conventional CBD or CBG extracts. However, this may soon change in light of this new research.
Here are 5 tips for finding products that contain CBDA & CBGA:
1. Look For “Raw,” Full-Spectrum Hemp Extracts
Raw cannabinoid extracts are hard to find, but the companies that are selling them usually make it very clear what you’re working with because of all the hard work that goes into producing and maintaining these products.
You’ll usually see terms like “raw hemp extract,” “CBDA,” or “CBGA” listed directly on products made with these ingredients (as opposed to just “CBD” or “CBG”).
→ Check out our list of high-potency raw CBDA oils.
2. Check the CBDA & CBGA Levels on Lab Tests Before You Buy
The only way to prove the products you’re using truly contain raw cannabinoids is to check the third-party lab tests.
In-house lab tests can determine this, too but shouldn’t be trusted. The cannabis industry has a track record of falsifying test reports, so it’s better to look for companies that use independent testing facilities instead.
Related: List of Scam CBD Companies to Watch Out For.
Example of a third-party lab test demonstrating CBDA content:
3. Avoid Products Intended For Smoking or Vaping
As mentioned already, if you have to heat your cannabinoids for any reason, they’ll lose the effectiveness of cannabinoids against COVID-19, as displayed in this study.
This is important to remember because there are some companies selling CBDA vape oils, pastes, and CBDA-rich hemp flower. None of these products should be smoked or vaped if you want the benefits of these cannabinoids on immunity.
Instead, look for oils or capsules. Gummies are sometimes okay, but the curing process will invariably decarboxylate at least some of the CBDA and CBGA. Even under ideal circumstances, around 15–20% of the CBDA and CBGA will decarboxylate by the time the gummies are ready to use.
4. Check The Date of Manufacture
Decarboxylation of cannabinoids occurs from exposure to heat, but it can also happen over time. Cannabinoids that have been sitting on a shelf for several months will gradually start to decarboxylate on their own — thus reducing their effectiveness for blocking SARS-CoV-2.
Look for products that come directly from the manufacturer and are less than 6-months old.
Resellers will often place large orders from manufacturers to increase profit. The problem with this is that if they don’t sell everything right away, products can end up sitting on store shelves for months at a time. Exposure to artificial lighting or heating can cause the CBDA and CBGA levels to drop even faster.
5. Keep Your Raw Cannabinoid Products Refrigerated
Once you’ve ordered your raw hemp oil, it’s important to store them correctly to limit further decarboxylation. You can keep oils, gummies, capsules, and resins in the fridge to slow the process and maintain the immune-boosting benefits for longer.
In general, you can expect to maintain over 80% of the original CBDA and CBGA levels of CBD oils kept in the fridge for about 6–8 months, but you should try and use them up more quickly if you can.

Other Herbs That (May) Act as Cell-Entry Inhibitors for SARS-CoV-2
Cannabinoids aren’t the first phytochemicals found to (potentially) inhibit SARS-CoV-2 from infecting the cell, and they certainly won’t be the last.
In fact, the same team credited with discovering these effects from cannabinoids has examined other plants as well. So far, the Oregon State University lab has screened compounds in such plants as wild yam, hops, red clover, and licorice.
Other labs have been conducting similar research for the last two years, and similar research took place during the first SARS-CoV-1 outbreak in 2002.
Here’s a brief roundup of some of the other compounds found in nature that have been shown to offer comparable cell-entry inhibiting actions.
1. Finger Root
(Boesenbergia rotunda)
Finger root is a culinary herb used in China and other countries located within Southeast Asia, where it grows naturally.
A recent study published at the end of 2020 reported an extract from finger root, called panduratin A, successfully suppressed the infectability of SARS-CoV-2 in human epithelial cells [9]. This research suggested an inhibitory action at both the pre-entry and post-infection stages.
2 Licorice Root
(Glycyrrhiza spp.)
Van Breeman has already been studying a compound from licorice called lichalcone A for several years and has since run several assays examining the potential antiviral actions of three separate species of licorice against SARS-CoV-2. However, the team has yet to publish their findings from this research. It’s likely the team moved to publish their work on cannabinoids first but will hopefully publish more findings throughout the rest of 2022.

Other studies have suggested another ingredient in licorice may offer protection from COVID-19.
Glycyrrhizin, a saponin responsible for the intensely sweet flavor of licorice, was found to bind to the ACE2 receptors on human cells [8] — potentially preventing the SARS-CoV-2 virus from being able to use them to infect the cell.
3. Houttuynia
(Houttuynia cordata)
Houttuynia has a long history of use in traditional medicine for treating different kinds of infections, including viral infections. It was highly popular in China during the first SARS outbreak in 2002.

A study published in 2008 pointed out three key mechanisms that could explain the powerful antiviral activity of this herb [5]:
- Houttuynia increases the secretion of IL-2 and IL-10, which are key immunoglobulins used to combat viral infection.
- Houttuynia increases CD4+ and CD8+ T-cells, which are integral to our adaptive immune response and are necessary for fighting viral infection.
- Houttuynia inhibited two key enzymes involved with the SARS-CoV-1 functionality (3CLPro and RNA-dependant RNA polymerase).
4. Elderberry
(Sambucus nigra)
Elder is already well known for its antiviral effects. It contains a series of lignans and terpenes that have been found effective at reducing the infectious potential of influenza A and B, human immunodeficiency virus (HIV), feline immunodeficiency virus (FIV), herpes simplex (HSV), and coronavirus in chickens.
One study discovered that an extract of Sambucus formosanaNakai strongly inhibited the replication of coronavirus NL63 — which is one of the primary coronaviruses responsible for the common cold [3].
Another study found that an extract of Sambucus nigra (black elderberry) reduced the severity of the infectious bronchitis virus (a strain of pathogenic chicken coronavirus) [4].
5. Bupleurum
(Bupleurum falciform)
Bupleurum is a traditional Chinese medicine herb mainly used for treating disorders of the liver.
Recently, a group of compounds present in bupleurum called saikosaponins were found to provide potent antiviral effects [6]. So far, these saikosaponins have been shown to inhibit HSV, hepatitis B, measles, and HCoV-22E9 [7] (one of the most common coronaviruses responsible for the common cold).

Much like CBDA and CBGA, saikosaponins are thought to interfere with the virus’s ability to enter the cell by binding and deactivating the spike proteins on the outside of the viral envelope.
Final Thoughts: Can Cannabis Help Protect Us Against COVID-19?
This study doesn’t offer any conclusive evidence that cannabinoids can prevent or treat COVID-19, but it did provide results that were promising enough to warrant further research.
So far, we know that CBDA and CBGA can prevent the ability of SARS-CoV-2 to infect cells in test tubes. We also have a mechanism of action for how this might work (binding and inhibition of key areas of the coronavirus spike proteins).
However, in vitro research isn’t strong enough to draw any clinical conclusions. It’s entirely possible that these effects won’t be replicated when tested in animal or human subjects. It’s also possible that the effective dose needed to achieve these benefits is simply too large to be of any practical value.
With that aside, if you’d like to apply the findings of this study, it’s important to use the right stuff.
This study showed us that only the raw, non-decarboxylated versions of CBD and CBG (CBDA and CBGA, respectively) offer this protection. This means you can’t get these benefits from smoking, vaping, or using decarboxylated cannabinoids of any kind.
Opt for raw, full-spectrum oils or extracts only. It’s also wise to double-check the lab tests before you buy to ensure the products you’re ordering truly contain the non-decarboxylated versions of CBD or CBG.
References
- van Breemen, R. B., Muchiri, R. N., Bates, T. A., Weinstein, J. B., Leier, H. C., Farley, S., & Tafesse, F. G. (2022). Cannabinoids Block Cellular Entry of SARS-CoV-2 and the Emerging Variants. Journal of natural products.
- Wakshlag, J. J., Schwark, W. S., Deabold, K. A., Talsma, B. N., Cital, S., Lyubimov, A., … & Zakharov, A. (2020). Pharmacokinetics of cannabidiol, cannabidiolic acid, Δ9-tetrahydrocannabinol, tetrahydrocannabinolic acid and related metabolites in canine serum after dosing with three oral forms of hemp extract. Frontiers in Veterinary Science, 7, 505.
- Weng, J. R., Lin, C. S., Lai, H. C., Lin, Y. P., Wang, C. Y., Tsai, Y. C., … & Lin, C. W. (2019). Antiviral activity of Sambucus FormosanaNakai ethanol extract and related phenolic acid constituents against human coronavirus NL63. Virus research, 273, 197767.
- Chen, C., Zuckerman, D. M., Brantley, S., Sharpe, M., Childress, K., Hoiczyk, E., & Pendleton, A. R. (2014). Sambucus nigra extracts inhibit infectious bronchitis virus at an early point during replication. BMC veterinary research, 10(1), 1-12.
- Lau, K. M., Lee, K. M., Koon, C. M., Cheung, C. S. F., Lau, C. P., Ho, H. M., … & Fung, K. P. (2008). Immunomodulatory and anti-SARS activities of Houttuynia cordata. Journal of ethnopharmacology, 118(1), 79-85.
- Bermejo, P., Abad, M. J., Díaz, A. M., Fernández, L., De Santos, J., Sanchez, S., … & Irurzun, A. (2002). Antiviral activity of seven iridoids, three saikosaponins and one phenylpropanoid glycoside extracted from Bupleurum rigidum and Scrophularia scorodonia. Planta medica, 68(02), 106-110.
- Cheng, P. W., Ng, L. T., Chiang, L. C., & Lin, C. C. (2006). Antiviral effects of saikosaponins on human coronavirus 229E in vitro. Clinical and Experimental Pharmacology and Physiology, 33(7), 612-616.
- Luo, P., Liu, D., & Li, J. (2020). Pharmacological perspective: glycyrrhizin may be an efficacious therapeutic agent for COVID-19. International Journal of antimicrobial agents, 55(6), 105995.