Evidence based
What is THCC? How is it Different From THC?
THCC is a non-psychoactive compound found in cannabis pollen. Learn how this novel cannabinoid may offer stronger pain relief for certain conditions than CBD.
There are many different forms of THC. The most common is delta 9 THC — which is the active ingredient in marijuana that makes users feel high.
While THCC is a form of THC, its effects are more similar to CBD (cannabidiol). It’s non-psychoactive and has shown particular promise as a treatment for chronic nerve and osteoarthritis pain.
This cannabinoid has been known for well over a decade, but there’s very little research available exploring its effects.
Here, you’ll learn all about THCC and why this unique cannabinoid offers promise as a new, more powerful non-psychoactive painkiller for certain conditions than CBD.
What is THCC?
THCC (Δ9-tetrahydrocannabiorcol) is a naturally occurring cannabinoid found in the pollen of the cannabis plant. This means this cannabinoid comes from the male cannabis plants rather than the female plants like most other cannabinoids.
Currently, the only commercial application of the male plants is breeding and the production of hemp seeds.
THCC is not well studied, so it’s unclear where this cannabinoid falls in terms of safety and efficacy. There’s been some interesting preliminary research that suggests this cannabinoid could be a powerful painkiller and neuroregulator.
What Are the Effects of THCC?
THCC is non-psychoactive but may offer powerful analgesic effects for certain types of pain.
Preliminary studies have shown this cannabinoid doesn’t have a strong affinity for the CB1 or CB2 receptors [1]. Therefore, THCC doesn’t produce the characteristic high from other forms of THC, such as delta 9 THC, delta 8 THC, THCV, THCP, or THC-O. THCC is more similar to CBD than it is to THC.
What makes this cannabinoid unique is its ability to bind to the vanilloid receptors (TRPA1). These receptors are intimately involved in the regulation of pain, as well as other functions like body temperature regulation and nerve transmission.
A study published in Nature in 2011 explored the potential painkilling activity of THCC against another known TRPA1 agonist, acetaminophen (AKA, Aspirin) [2]. The study concluded that THCC and other TRPA1-mediators are promising candidates for new forms of analgesic medicines.
What is TRPA1 & What is its Significance?
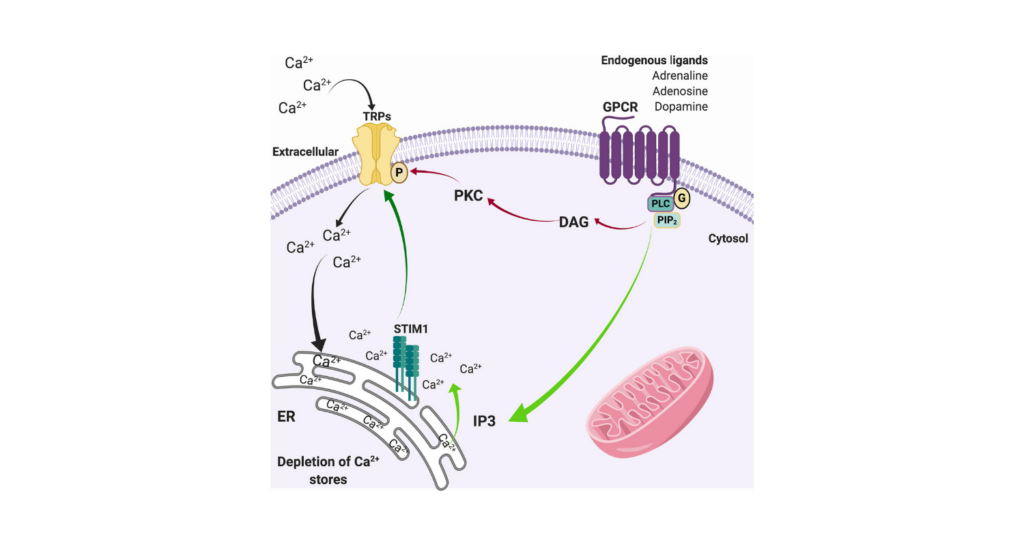
TRPA1 is a protein structure that forms on cell membranes. It acts as a receptor and also forms ion channels that transmit information into the cell when certain conditions are met [3].
This receptor acts as a sensor for detecting noxious stimuli and converting that signal into pain and inducing a cascade of other effects such as tearing, coughing, sneezing, and inflammation.
TRPA1 is often referred to as the “wasabi receptor” or the “capsaicin receptor,” — which gives you a clue as to the type of noxious chemicals this receptor is designed to detect.
Whenever you eat foods like chili, mustard, or wasabi or are exposed to other noxious chemicals like tear gas or pepper spray, your body’s reaction relies on the activation of the TRPA1 receptors. You feel the urge to cough, inflammation causes warmth and pain, and you start to sneeze or feel your nose start to run.
There’s also some indication this receptor serves as a sensor for noxious hot or cold temperatures.
Ultimately, the role of TRPA1 as a potential new pain-management pathway looks promising, but there’s still a lot we don’t know. Thanks to dedicated researchers at UCSF, including David Julius, Yifan Cheng, Candice Paulsen, Jean-Paul Armache, David Agard, and others, we’re starting to make some real headway in the therapeutic potential of this unique receptor.
Can THCC Manage Chronic Pain?
There isn’t enough research to make any claims, but the current evidence suggests THCC as a promising candidate for treating certain types of pain.
The ability of this compound to target the TRPA1 receptors makes it especially promising.
TRPA1 mediators are currently being explored as a new target for the next generation of painkillers [10] — especially neuropathic pain, chronic inflammatory pain, and osteoarthritis-related pain.
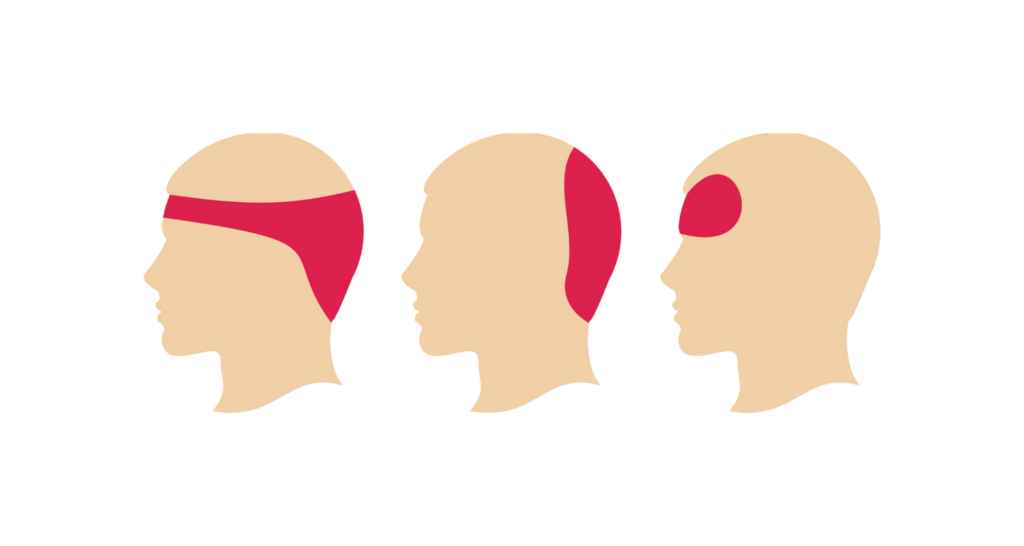
1. THCC For Migraine Headaches
Migraine headaches are still poorly understood by modern medicine. While there are several leading theories, no specific cause has been established. The mechanism of action for migraines is thought to involve an abnormal release of serotonin, changes in cerebral blood flow, or a spasm of the blood vessels that feed blood to the brain.
There are also some well-established triggers for the cascade of effects that lead to migraine headaches. Exposure to cigarette smoke, various aromas, medications, and a compound called glyceryl trinitrate are all examples of triggers for migraine headaches.
Some studies suggest the reason these triggers cause migraine attacks is because they activate the TRPA1 receptors. Additionally, several of the effective treatment options available today for treating migraines work by desensitizing or blocking the action of TRPA1 [9].
While THCC has yet to be studied for this specific application, its potent TRPA1-mediating activity makes it a promising candidate for future migraine treatment and prevention.
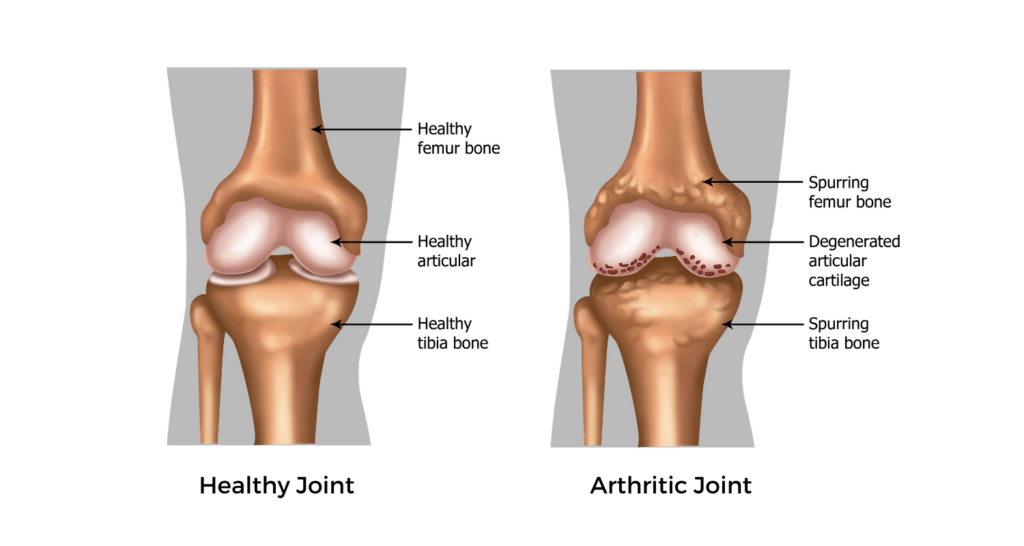
2. THCC For Osteoarthritis Pain
The role of TRPA1 and osteoarthritis pain is particularly interesting. Current evidence suggests the TRPA1 receptor is involved with the pain originating from the inflamed chondrocytes in arthritic joints [8].
TRPA1 mediators, such as THCC, may provide a new form of treatment for managing osteoarthritis pain directly, as well as through a reduction in pain hypersensitivity that often forms with chronic pain conditions.
3. THCC For Chemotherapy-Induced Pain
It’s common for chemotherapeutic medication to induce a certain type of nerve pain called allodynia. This condition makes people extremely sensitive to touch as well as changes in temperature.
There are many chemotherapy medications that can have this effect, but some of the most notable are paclitaxel and oxaliplatin.
TRPA1 activation is thought to be the primary cause of this form of nerve pain [7], so it’s possible that TRPA1 mediators like THCC could provide direct relief for this form of chemotherapy pain. More research is needed to understand this effect in more detail.
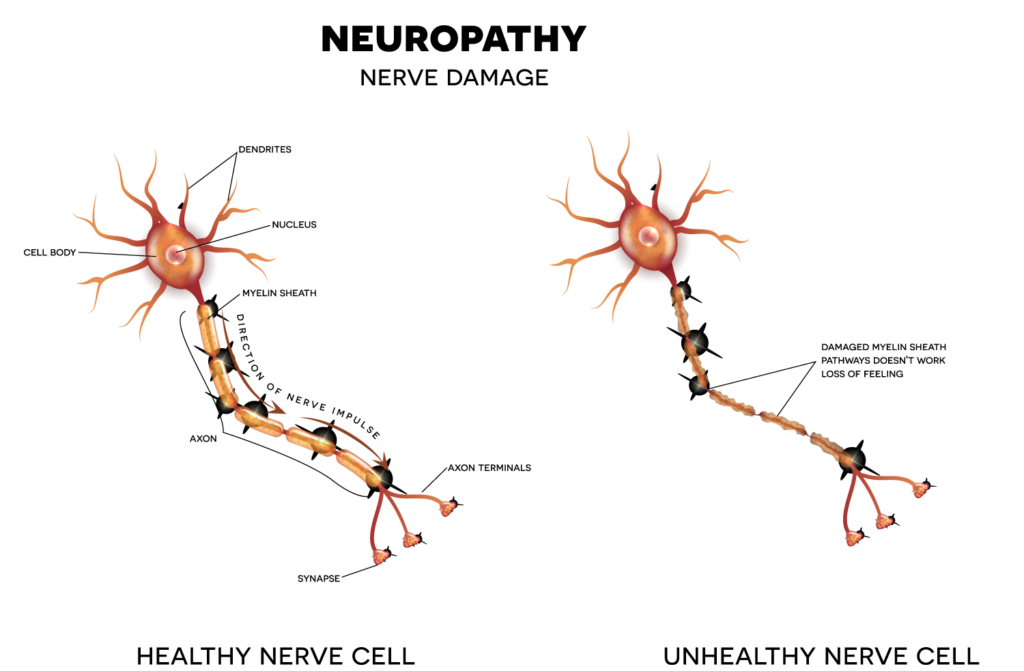
4. THCC For Diabetic Neuropathic Pain
Diabetic neuropathy is a condition in which elevated blood sugar levels (as a result of diabetes mellitus) causes damage and destruction to the cells in the surface of the skin, especially in the toes and fingers. As the nerve cells are damaged along with surrounding tissue, it causes intense, persisting pain.
A recent study found that TRPA1 mediators were able to attenuate diabetic neuropathy-induced pain in rats [6]. The effect was especially remarkable in TRPA1 mediators with action on the TRPA1 receptors located in the spinal cord rather than strictly in the affected area.
THCC hasn’t been studied for this effect directly, but current evidence suggests it interacts with both the peripheral TRPA1 and spinal TRPA1 receptors.
5. THCC For Sleep-Deprivation-Induced Pain Hypersensitivity
Studies have shown loss of sleep can make us more sensitive to pain [4].
This is a bit of a catch-22.
More pain = less sleep; and less sleep = more pain.
THCC has not been studied for this effect specifically — but similar TRPA1 mediators have been shown to reverse sleep deprivation-induced hypersensitivities to pain in rats [5].

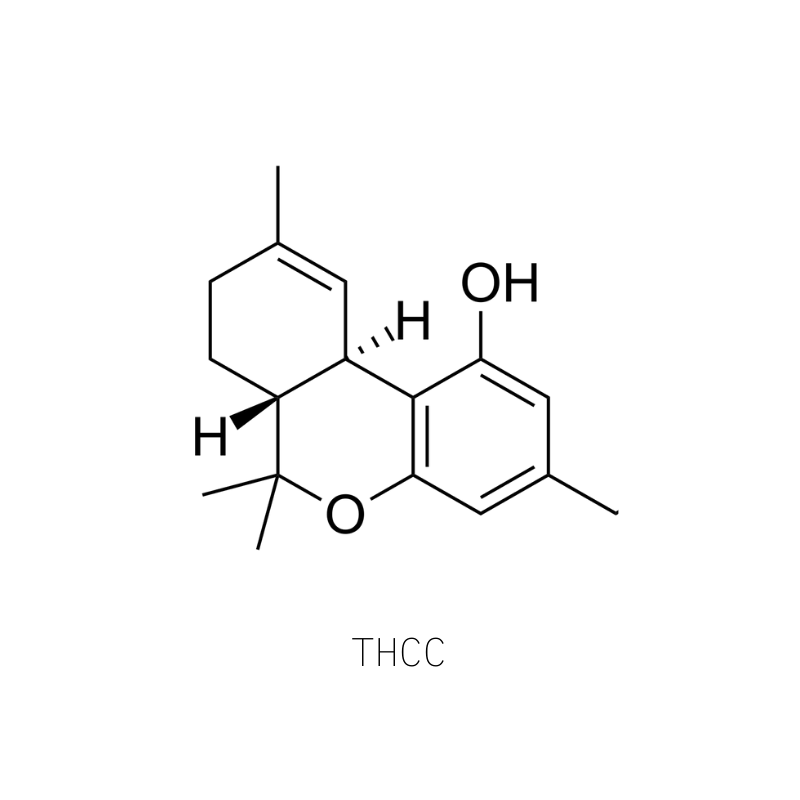
Why Isn’t THCC Psychoactive?
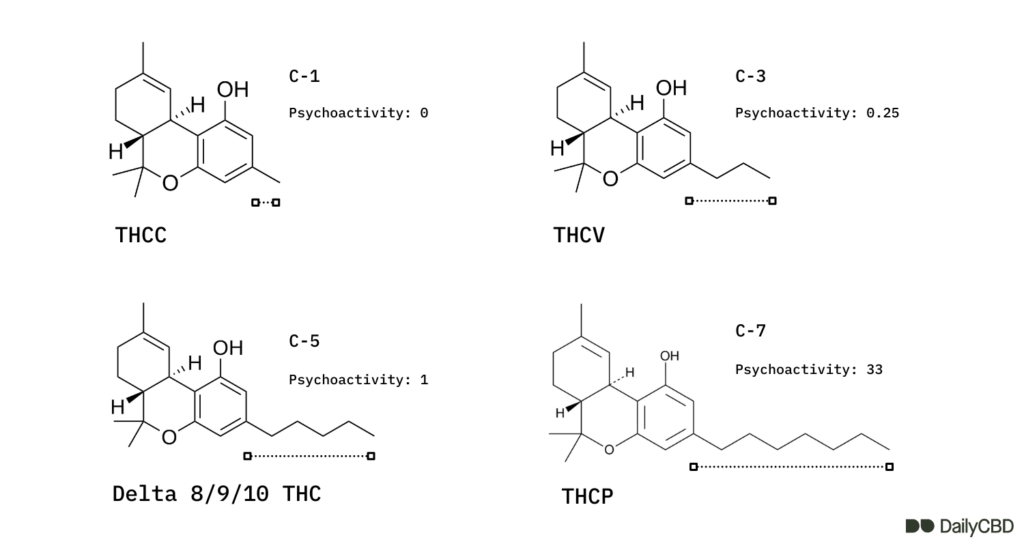
Structurally, THCC is very similar to THC. The only difference is the number of carbon atoms attached to its functional side chain. Instead of having five carbons, like THC, it has 1. This is why THCC is sometimes referred to as THC-C1.
The potency of THC largely relies on the number of carbons in its side chain:
- As the baseline, THC has 5 carbons in this particular chain.
- THCV has 3 carbons, and has about 25% the potency of THC.
- THCP has 7 carbons and is anywhere from 5 to 30 times as strong as THC.
- THCC has 1 carbon and doesn’t possess any psychoactive effects.
Studies exploring the effects of THC with different side-chain lengths have concluded that there need to be at least 3 carbons in this chain for the molecule to exert any psychoactive effects through the endocannabinoid system (ECS).
What’s The Future of THCC?
As more research is published every year on the effects of novel cannabinoids like THCC, it’s likely we’re going to see an explosion of new cannabinoid-based medicines and supplements enter the market in the next couple of years.
The unique ability for THCC to interact with the TRPA1 receptors may make this one of the more useful products in the coming years for certain neurological conditions or nerve pain.
THCC is comparable to CBD in its painkilling effects but may provide more specific relief to certain kinds of pain — such as peripheral diabetic neuropathy, traumatic neuropathy, chemotherapy-induced neuropathy, osteoarthritis, postoperative surgical pain, migraine headaches, or pain from bacterial infections.
We have yet to find a reputable source for this cannabinoid but will update this page when we do.
Watch this space.
References
- Bow, E. W., & Rimoldi, J. M. (2016). The structure-function relationships of classical cannabinoids: CB1/CB2 modulation. Perspectives in medicinal chemistry, 8, PMC-S32171.
- Andersson, D. A., Gentry, C., Alenmyr, L., Killander, D., Lewis, S. E., Andersson, A., … & Zygmunt, P. M. (2011). TRPA1 mediates spinal antinociception induced by acetaminophen and the cannabinoid Δ 9-tetrahydrocannabiorcol. Nature communications, 2(1), 1-11.
- Guimaraes, M. Z., & Jordt, S. E. (2006). 11TRPA1: a sensory channel of many talents. TRP ion channel function in sensory transduction and cellular signaling cascades, 151.
- Lautenbacher, S., Kundermann, B., & Krieg, J. C. (2006). Sleep deprivation and pain perception. Sleep medicine reviews, 10(5), 357-369.
- Wei, H., Koivisto, A., Saarnilehto, M., Chapman, H., Kuokkanen, K., Hao, B., … & Pertovaara, A. (2011). Spinal transient receptor potential ankyrin 1 channel contributes to central pain hypersensitivity in various pathophysiological conditions in the rat. PAIN®, 152(3), 582-591.
- Wei, H., Koivisto, A., Saarnilehto, M., Chapman, H., Kuokkanen, K., Hao, B., … & Pertovaara, A. (2011). Spinal transient receptor potential ankyrin 1 channel contributes to central pain hypersensitivity in various pathophysiological conditions in the rat. PAIN®, 152(3), 582-591.
- Chen, Y., Yang, C., & Wang, Z. J. (2011). Proteinase-activated receptor 2 sensitizes transient receptor potential vanilloid 1, transient receptor potential vanilloid 4, and transient receptor potential ankyrin 1 in paclitaxel-induced neuropathic pain. Neuroscience, 193, 440-451.
- Moilanen, L. J., Hämäläinen, M., Nummenmaa, E., Ilmarinen, P., Vuolteenaho, K., Nieminen, R. M., … & Moilanen, E. (2015). Monosodium iodoacetate-induced inflammation and joint pain are reduced in TRPA1 deficient mice–potential role of TRPA1 in osteoarthritis. Osteoarthritis and cartilage, 23(11), 2017-2026.
- Benemei, S., Fusi, C., Trevisan, G., & Geppetti, P. (2014). The TRPA1 channel in migraine mechanism and treatment. British journal of pharmacology, 171(10), 2552-2567.
- Koivisto, A., Jalava, N., Bratty, R., & Pertovaara, A. (2018). TRPA1 antagonists for pain relief. Pharmaceuticals, 11(4), 117.