Does CBD Interact With Warfarin (Coumadin)?
CBD & warfarin (Coumadin) carry a moderate to high risk of interaction. Speak to your doctor about CBD if you’ve been prescribed blood thinners.
Warfarin (Coumadin) is an anticoagulant. It’s used to prevent clot formation in conditions such as deep vein thrombosis, pulmonary embolism, to prevent stroke, and as an adjunct treatment for angina and myocardial infarction.
Cannabidiol (CBD), a cannabinoid from hemp and marijuana plants, is a popular alternative treatment for pain, inflammation, anxiety, insomnia, and as a general health supplement.
Is it safe to mix blood thinners like warfarin with CBD or other cannabinoids?
Does CBD Interact With Warfarin (Coumadin)?
Yes. CBD may interact with warfarin (Coumadin). This combination is considered moderate to high risk of interaction and should be avoided unless otherwise specified by your doctor.
This combination may slow the breakdown and elimination of warfarin, leading to increased serum levels of both substances over time. If serum concentrations become too high, side effects will result — some of which are severe and require medical attention (such as internal bleeding).
There are two main ways by which CBD can interact with warfarin:
A) Slowed Elimination (Metabolic Inhibitor)
Metabolic inhibition occurs when two drugs need the same enzymes to get metabolized. Hence, they end up competing against each other for the said enzymes. This action could result in slowing down the metabolism of one or both drugs.
Warfarin is metabolized by the CYP450 enzymes, mainly by CYP3A4 and CYP2C19, and less commonly by CYP1A22, CYP2D6, and CYP3A5.
These same enzymes metabolize CBD as well. Besides this, CBD is also capable of inhibiting these enzymes. So taking warfarin and CBD together could slow down the former’s metabolism.
This action could also lead to an excess accumulation of warfarin in the body, causing severe side effects such as bleeding, bruising, severe headaches, etc.
B) Increased Effect (Agonistic Interaction)
Agonistic interaction occurs when two drugs have similar effects on the body. When used together, both these drugs push on the same receptors or cause some effects in the same direction.
CBD can cause excess accumulation of warfarin in the body. It can also make it sustain for a longer time. It means warfarin would stay in the body for longer and become more potent. Hence, CBD could work as an agonist for warfarin as well. But this could also lead to heightened abilities of warfarin and cause more side effects as well.
Is It Safe to Take CBD & Warfarin (Coumadin) Together?
CBD and warfarin (Coumadin) are unlikely to result in serious side effects — however, this combination isn’t considered safe because of the severity of potential side effects should there be an interaction.
This combination could lead to an increase in the side effects of warfarin. Some recent studies have explored the potential interaction of these compounds [1]. Studies have shown high chances of a rise in the international normalized ratio (INR) of the users who are on long-term warfarin.
This means the blood may clot more slowly in users taking both these drugs, causing a tendency to bleed more easily. This could result in serious internal bleeding, bruising, or hemorrhage from relatively small injuries.
It is not recommended to take these two medicines together. Always consult your physician first before you decide to start CBD while on warfarin or any other blood thinner medications.
Your doctor may want to modify your dose of warfarin or CBD and may suggest taking both substances at least 2 hours apart.
If necessary, take only a minimal dose of CBD and always be wary of any abnormal side effects. In patients who are taking warfarin and have started CBD, it’s suggested to do regular laboratory tests, especially the INR test. If you experience any side effects, contact your medical practitioner at once.

Similar Medications: CBD & Blood Thinners
Warfarin is classified as an anticoagulant. CBD and most blood thinners share a similar risk of interaction and side effects.
Here’s a list of similar medications that share a similar level of risk when combined with CBD:
- Apixaban (Eliquis)
- Dabigatran (Pradaxa)
- Enoxaparin (Lovenox)
- Heparins
- Rivaroxaban (Xarelto)
- Clopidogrel (Plavix)
Is CBD A Viable Alternative to Warfarin (Coumadin)?
CBD is not a viable alternative to warfarin. These medications work through entirely different mechanisms and are used to treat different conditions altogether.
Some studies show that cannabis, the base ingredient of CBD, may have some anticoagulant properties [2]. A study performed on obese rats demonstrated that cannabis displays some anticoagulant activity.
It also showed that the cannabinoids cannabinol (CBN) and delta 9 tetrahydrocannabinol (THC) might also have anticoagulant abilities.
However, these effects are substantially weaker than the anticoagulant effects of warfarin and are therefore not suitable as a substitute for this prescription medication.
What is Warfarin (Coumadin)?
Warfarin, the generic name of the drug Coumadin, is a type of anticoagulant or blood thinners.
It’s a vitamin K antagonist that can decrease the rate of clotting of blood in the body.
Warfarin is used to treat and prevent blood clots in several conditions such as deep vein thrombosis, pulmonary embolism, etc. It’s used as a preventative for patients at risk of a stroke (such as those diagnosed with atrial fibrillation, valvular heart disease, or artificial heart valves).
Warfarin is also used to reduce the risk of death in patients with recurrent myocardial infarction (heart attack), stroke, and systemic embolism.
Coumadin is a prescription drug approved for use by the FDA in 2007.
Warfarin Specs:
| Drug Name | Warfarin |
| Trade Names | Coumadin, Jantoven, Warf, Warfin, Farin, Fargem, Warco |
| Classification | Anticoagulant |
| CYP Metabolism | Major: CYP3A4 & CYP2C19. Minor: CYP1A22, CYP2D6, & CYP3A5 |
| Interaction With CBD | Metabolic inhibitor, agonistic |
| Risk of Interaction | High |
What Does Warfarin Do?
Warfarin is an anticoagulant. It was originally produced as rat poison, but its anticoagulant ability proved to be a valuable asset in treating hypercoagulable conditions. It was formally approved for human use in 1954 to treat blood clots.
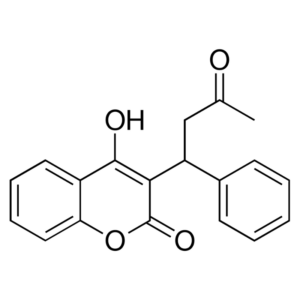
Warfarin can disrupt the coagulation cascade and stop clot formations. It is a vitamin K antagonist that inhibits the production of vitamin K by using an enzyme called vitamin K epoxide reductase.
Warfarin blocks the liver from using vitamin k to make clotting factors. It can thin out the blood so that clotting time increases. It takes about three days for its abilities to take full effect. After this, however, it can take a few weeks to get a stable level of warfarin in the blood and get the body to settle on the correct dosage.
Warfarin stops the synthesis of biologically active forms of clotting factors II, VII, IX, and X. It also inhibits the synthesis of regulatory factors protein C, protein S, and protein Z. It does this by competitively inhibiting the vitamin K epoxide reductase complex 1 (VKORC1), an enzyme essential for activating the vitamin K in the body.
The precursors of these factors need their glutamic acid residues to undergo gamma-carboxylation. Gamma carboxylation is required so that the coagulation factors can bind to phospholipid surfaces inside blood vessels. The enzyme that allows the carboxylation of glutamic acid is gamma-glutamyl carboxylase.
Carboxylation reaction is possible only if the carboxylase enzyme converts vitamin k hydroquinone (a reduced form of vitamin k) to vitamin k epoxide. The vitamin k epoxide gets recycled back to vitamin K and vitamin k hydroquinone by another enzyme called vitamin k epoxide reductase.
Warfarin inhibits vitamin k epoxide reductase. This action leads to the diminishing of the available vitamin K and vitamin K hydroquinone in the tissues, which decreases the carboxylation activity of the glutamyl carboxylase. The drug works by inhibiting the formation of Vitamin K and making coagulation factors unable to work.
When this occurs, the coagulation factors are no longer carboxylated at some glutamic acid residues and are incapable of binding to the endothelial surface of blood vessels. This makes them biologically inactive. Hence, the coagulation factors are still being produced but have decreased ability to work.
Warfarin needs to be adjusted according to individual needs, and the dosage may be increased or decreased depending on the response of the treatment. Dosing and adjusting warfarin can be complicated as it is known to interact with many medications. Regular laboratory tests, including international normalized ratio (INR), are mandatory after starting warfarin to monitor the coagulation levels in the body.
The risk factors of excess bleeding on using warfarin can be found in patients with high intensity of anticoagulation or high INR, age of over 65 years, highly variable INR, patients with a history of gastrointestinal bleeding, high blood pressure, serious heart disease, anemia, and renal insufficiency.
Warfarin is contraindicated in some conditions such as pregnancy, recent major surgery, thrombocytopenia, coagulation defects, decompensated liver disease, known hypersensitivity, and hemorrhagic tendencies.
Side Effects of Warfarin
- Severe bleeding such as heavy menstrual bleeding and internal hemorrhage
- Bleeding from gums, nosebleeds
- Easy bruising
- Red or brown urine
- Black or bloody stool
- Severe headache
- Stomach pain
- Joint pain
- Joint swelling or discomfort
- Vomiting blood or coffee-ground like materials
- Coughing up blood
- Abnormal bruising
- Dizziness
- Blood dyscrasias
- Hepatitis
- Weakness
- Vision changes
- Intracranial hemorrhage
- Lethargy
- Hypersensitivity
- Purple toe syndrome
- Renal injury
- Taste disturbance
- Flatulence
- Hair loss
- Intraocular hemorrhage
- Warfarin necrosis
- Osteoporosis
- Valvular and vascular calcification
Other Names For Warfarin (Coumadin)
Warfarin is sold under many different names. All share the same risk and potential interactions.
Other names for warfarin include:
- Jantoven
- Warf
- Marevan
- Farin
- Fargem
- Warco
- Warfin

Key Takeaways: Is it Safe to Take Warfarin With CBD?
CBD carries a moderate to high risk of interaction with warfarin. The severity of this interaction can be life-threatening.
It can decrease its rate of metabolism, make it more potent, have a longer duration of action, and increase the chances of experiencing side effects. Therefore, it’s not recommended to take them together unless advised by your prescribing medical practitioner.
If needed, use only a minimal amount of CBD and always be on the lookout for any side effects.
References
- Grayson, L., Vines, B., Nichol, K., & Szaflarski, J. P. (2018). An interaction between warfarin and cannabidiol, a case report. Epilepsy & behavior case reports, 9, 10.
- Coetzee, C., Levendal, R. A., Van de Venter, M., & Frost, C. L. (2007). Anticoagulant effects of a Cannabis extract in an obese rat model. Phytomedicine, 14(5), 333-337.
Signup to our newsletter
Be the first to know about our newest arrivals and special offers!