Does CBD Interact With Fosinopril (Monopril)?
CBD can interact agonistically with the antihypertensive fosinopril, causing an increase in potency and side effects, but is this dangerous?
Fosinopril is a drug used in treating hypertension. It belongs to the angiotensin-converting enzyme (ACE) inhibitors class but is also used to treat congestive heart failure and chronic renal failure.
There is a possibility of adverse reactions if you use fosinopril while you are on cannabidiol (CBD) or vice versa.
This interaction could cause an increased potency in one or both the drugs, leading to some unwanted and possibly severe side effects.

Does CBD Interact With Fosinopril (Monopril)?
Yes. CBD can interact with fosinopril. Both drugs have hypotensive actions — taking them together could cause sudden low blood pressure, headaches, dizziness, fainting, and nausea.
CBD may also interfere with the body’s ability to metabolize Monopril — altering blood levels and potentially leading to side effects.
The level of risk associated with this interaction is considered moderate.
Caution: Always speak to a doctor before taking CBD if you’re taking any prescription medications.
A. CBD Can Increase Fosinopril’s Effects On the Body (Agonistic Interaction)
Fosinopril and CBD may have an agonistic interaction with each other. Agonistic interaction is where two drugs have similar effects on the body, making them more pronounced.
Fosinopril decreases blood pressure by inhibiting the angiotensin-converting enzyme (ACE). This prevents the conversion of angiotensin I into angiotensin II, causing vasodilation and, thus, a decrease in blood pressure.
On the other hand, CBD can also decrease blood pressure by acting on the endocannabinoid receptors present in the blood vessels.
Since both these drugs are antihypertensive, taking them together may cause a rapid decrease in blood pressure, causing it to go lower than normal.
B. CBD May Slow Down Fosinopril’s Metabolization (Metabolic Competition)
There is a possibility of metabolic inhibition when consuming CBD and fosinopril.
Cytochrome enzymes are responsible for metabolizing most substances in the body. We don’t know the exact enzyme that metabolizes fosinopril, but most ACE inhibitors are partially metabolized by the CYP3A4 enzyme [1].
CYP3A4 is one of the enzymes that metabolizes CBD too.
When two substances use the same enzyme for metabolism, metabolic inhibition can occur, causing both substances to compete against each other for the enzymes.
Consuming CBD and fosinopril together could cause them to compete against each other, leading to a slowdown in their metabolism, overaccumulation, and more side effects.
Similar Medications: CBD & ACE Inhibitors
Fosinopril is an angiotensin-converting enzyme inhibitor. CBD and ACE inhibitors all share similar risks for interactions and side effects.
Here’s a list of similar medications that share a similar level of risk when combined with CBD:
- Benazepril hydrochloride (Lotensin)
- Captopril (Capoten)
- Enalapril maleate (Vasotec)
- Lisinopril (Prinivel & Zestril)
- Moexipril (Univasc)
- Perindopril (Aceon)
- Quinapril Hydrochloride (Accupril)
- Ramipril (Altace)
- Trandolapril (Mavik)
Is It Safe to Take CBD & Fosinopril (Monopril) Together?
CBD and fosinopril may be safe to take in minimum dosage for a short time as this can help prevent the drugs from accumulating in the body. Since they have a moderate level of interaction, a high dosage for a longer period may become dangerous.
As both have antihypertensive properties, long-term usage could cause problematic side effects like headaches, fainting, dizziness, low blood pressure, etc.
Never take these medications without consulting your prescribing physician first, and always be wary of any abnormal side effects. If you encounter anything unusual while taking these medications together, get medical help immediately.

Is CBD a Viable Alternative to Fosinopril (Monopril)?
CBD (cannabidiol) cannot be considered a viable replacement for antihypertensive drugs. It has antihypertensive properties but may not be adequate for use in severe cases.
CBD can release nitric oxide by acting on the CB1 receptors of the endothelium. This can help lower blood pressure; nitric oxide release can cause blood vessels to dilate [2].
Tachycardia due to various reasons may be a symptom of high blood pressure. One study showed that CBD could decrease high blood pressure in users who also have tachycardia [3].
CBD has antioxidative and anti-inflammatory properties too. These may help treat the inflammatory conditions that cause high blood pressure [4].
Hence, CBD has the potential to be a good adjunct and may even work as a mild antihypertensive. However, its use as a perfect alternative to antihypertensives may not be feasible just yet.
What is Fosinopril (Monopril)?
Fosinopril is an antihypertensive of the angiotensin-converting enzyme (ACE)inhibitor. It is used for hypertension and congestive heart failure and slows the progression of renal disease in hypertensive diabetics. One of its commonly used brand names is Monopril.
It is FDA-approved and available as a prescription drug.
Fosinopril (Monopril) Specs:
| Drug Name | Fosinopril |
| Trade Name | Monopril, Focinace, Fovas |
| Classification | Angiotensin-converting enzyme (ACE) inhibitor |
| CYP Metabolism | CYP3A4 |
| Interaction With CBD | Agonistic, Metabolic competition |
| Risk of Interaction | Moderate |
Other Names For Fosinopril (Monopril)
Fosinopril is sold under a few different names. All share the same risk and potential interactions.
Other names for fosinopril (Monopril) include:
- Focinace
- Fovas
What Does Fosinopril (Monopril) Do?
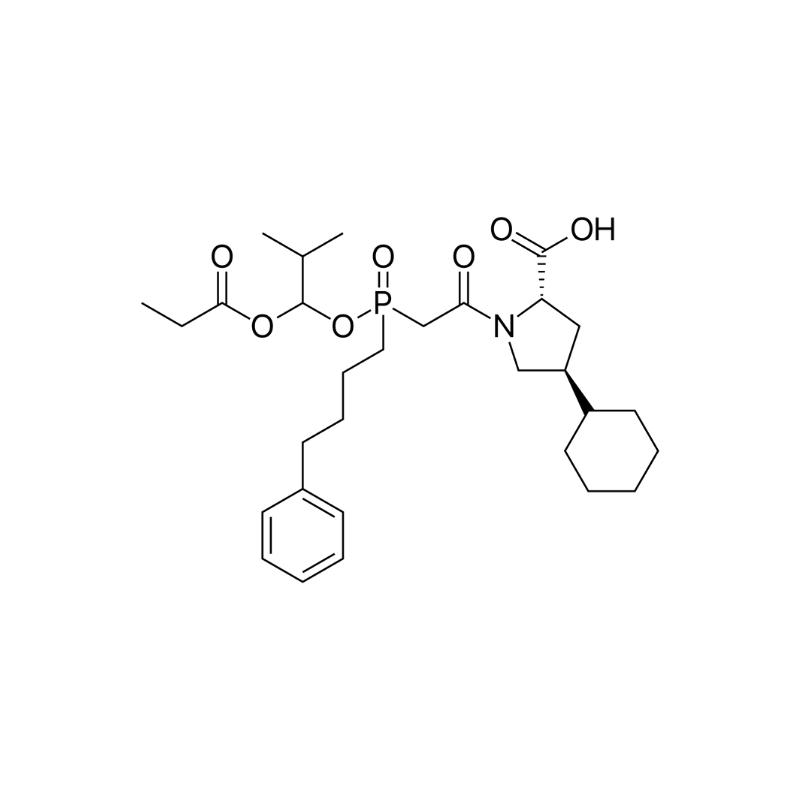
Fosinopril is a phosphinic acid-containing ester prodrug. Once in the body, it gets hydrolyzed to its active metabolite fosinoprilat. This fosinoprilat works by inhibiting the ACE enzyme, which is responsible for converting angiotensin I (ATI) to angiotensin II(ATII). ATII is responsible for the renin-angiotensin-aldosterone system (RAAS).
RAAS mechanism can control and regulate blood circulation, water, and electrolyte balance. Some actions like sympathetic stimulation, less blood pressure, or less blood flow into the kidney cause a substance called renin to be released.
Renin converts the circulating angiotensinogen in the bloodstream into ATI, which then further converts it into ATII by ACE. ATII stimulates the secretion of aldosterone from the adrenal cortex, causing an increase in sodium and water reabsorption, which leads to a rise in blood pressure.
ATII can also stimulate the secretion of antidiuretic hormones (ADH) or vasopressin from the posterior pituitary gland. This action allows further reabsorption of water from the kidneys. ATII also constricts the arteries, causing a rise in blood pressure.
AII can cause negative effects on the cardiovascular system after some detrimental events such as heart failure and myocardial infarction. AII causes arterial vasoconstriction and hypertension, increasing afterload and resistance.
Fosinopril slows this down by competing against angiotensin I for binding at the angiotensin-converting enzyme.
Fosinopril increases exercise tolerance and reduces the symptoms of heart failure, such as dyspnea, need for diuretics, and hospitalization.
Fosinopril was specifically designed for users with renal impairment. It has a half-life of 12 hours, and it stays in the system for almost 24 hours.

Side Effects of Fosinopril (Monopril)
Fosinopril is contraindicated in pregnancy. It can affect the renin-angiotensin system in babies, causing oligohydramnios, and may even cause fetal death or injury.
It should not be used in users with:
- A history of hereditary or idiopathic angioedema
- With neprilysin inhibitors such as sacubitril
- Bilateral renal artery stenosis
Side effects of fosinopril (Monopril) include:
- Angioedema
- Aplastic anemia
- Arthralgia
- Cough
- Diarrhea
- Dizziness
- Fatigue
- Headache
- Hyperkalemia
- Hypersensitivity
- Interstitial nephritis
- Neutropenia
- Orthostatic hypotension
- Rash
- Vasculitis

Key Takeaways: Is it Safe to Take Fosinopril (Monopril) With CBD?
It may be safe to take fosinopril and CBD in a minimum dosage for a short time, but only under medical supervision.
These two drugs can have a moderate level of agonistic interaction, making the combination possibly dangerous.
Their interaction could cause a rapid drop in blood pressure, dizziness, headaches, and other, possibly severe, side effects.
Always take these two medications only after consulting your prescribing physician. Always take the correct dosage at the recommended time and never overdose.
References
- Sadovsky, R. (2002). Antihypertensive agents and cytochrome p450 interactions. American Family Physician, 65(11), 2356.
- Stanley, C. P., Hind, W. H., Tufarelli, C., & O’Sullivan, S. E. (2015). Cannabidiol causes endothelium-dependent vasorelaxation of human mesenteric arteries via CB1 activation. Cardiovascular Research, 107(4), 568-578.
- Jadoon, K. A., Tan, G. D., & O’Sullivan, S. E. (2017). A single dose of cannabidiol reduces blood pressure in healthy volunteers in a randomized crossover study. JCI insight, 2(12).
- Atalay, S., Jarocka-Karpowicz, I., & Skrzydlewska, E. (2020). Antioxidative and anti-inflammatory properties of cannabidiol. Antioxidants, 9(1), 21.
Signup to our newsletter
Be the first to know about our newest arrivals and special offers!