| Total CBD: | 750 mg |
| Potency: | 25 mg per Capsule |
| Cost per mg CBD: | $0.11 |
| Extract Type: | Full-Spectrum |
| THC Content: | <0.3% |

Evidence based
Can CBD Help with PCOS? Benefits, Dosage, & Side-Effects
Can CBD help with polycystic ovarian syndrome (PCOS)? What does the current research suggest?
We’ll explore this connection in more detail.
Polycystic ovarian syndrome (PCOS) affects roughly 10% of women in the United States. It’s one of the main causes of infertility in women in the Western world [1].
This chronic health condition is poorly understood by modern medicine — making it especially difficult to diagnose and treat. Pharmaceuticals used to manage this condition bring their own risk of side-effects.
This has prompted a lot of people to reach for a bottle of CBD oil instead.
Can CBD really be used to benefit PCOS?
Here’s what the research says.
Best CBD Oils For PCOS
- Royal CBD Oil — Best CBD Oil Overall
- Gold Bee CBD Oil — Best Organic CBD Oil
- CBDistillery CBD Oil — Best CBD Isolate Oil
- Lazarus Naturals CBD Oil — Best Entry-Level CBD Oil
- Endoca CBD Oil — Best CBD Oil For PCOS (Europe)
What Are The Benefits of CBD Oil For PCOS?
CBD primarily works by helping the body maintain homeostasis (balance).
This includes the balance of hormones, neurotransmitters, metabolism, and neurological activity — all of which are affected by PCOS.
When using CBD for PCOS, don’t expect anything to happen overnight. The changes are slow and gradual. The biggest changes happen over time the more often you use it.
It’s always wise to speak with a doctor about using CBD oil for any health condition before you start — especially if you’re using any other prescription medications.
The benefits of CBD oil for PCOS include:
- Regulates insulin & blood sugar levels
- Promotes weight loss
- Relieves anxiety & depression
1. Regulates Insulin & Blood Sugar Levels
Hyperinsulinemia is characterized by excessive insulin levels in the bloodstream — which has a lot of overlap with diabetes.
A recent study involving more than 4600 participants diagnosed with diabetes or prediabetes had their self-reported use of marijuana and fasting insulin levels compared (a marker for hyperinsulinemia). Researchers found that participants using marijuana on a regular basis had a 16% lower insulin resistance score than non-users [2].
Researchers in this study suggested CBD as one of the key compounds responsible for producing this effect through the modulation of CB1 receptors. Other studies have shown that by blocking CB1 receptors in animal models, insulin sensitivity was improved [3]. This suggests the endocannabinoid system and CB1 receptors play a critical role in the function of insulin.
The idea is that if we’re more sensitive to the effects of insulin, we’ll have greater blood sugar regulation and improved negative feedback control of insulin balance. This is important because of the correlation of insulin imbalance with PCOS.
2. Supports Weight Loss
Roughly 80 percent of PCOS sufferers are considered overweight [4]. There are a few reasons for this:
- Fatigue leading to less exercise
- Hyperinsulinemia and diabetes leading to excess fat production
- Genetic predispositions to increased weight
This suggests excess weight gain as a potential contributing factor to the underlying cause of PCOS. One of the key goals of treatment in overweight PCOS patients is to cut excess weight.
CBD may be useful for supporting weight loss in a few ways:
- Regulation of mitochondrial function to improve the burning of excess sugar and fat as energy [5].
- Reducing insulin resistance to improve blood sugar regulation and support beta-oxidation of fat [2]
- Reducing appetite to help lower calorie intake [6]

3. Relieves Anxiety & Depression
One of the main side-effects of PCOS is anxiety. This can result from stress caused by the discomfort of the condition itself, or issues involving the adrenal glands where stress hormones like cortisol are produced.
Anxiety is one of the most common reasons people are taking CBD supplements — and there’s a lot of research to back this up.
A double-blind, placebo-controlled study comparing the anti-anxiety effects of CBD to benzodiazepine anxiety medications concluded that “CBD [has] anxiolytic properties in human volunteers submitted to a stressful situation” [7].
Other studies investigating the immediate effects of CBD in the treatment of anxiety used a public speaking model to induce an anxious state in study participants. The study noted a dramatic improvement in anxiety scores compared to placebo control [8].
There are a few ways CBD provides relief from anxiety symptoms, with the most important being a potentiation of GABA in the brain [9,10], which is the primary inhibitory neurotransmitter.
When the brain becomes hyperactive it’s GABA that slows it back down again — preferably before reaching levels high enough to cause an anxiety attack.
What’s The Dose of CBD Oil For PCOS?
The correct dose of CBD will vary from one person to the next. Some people find they need a large dose to achieve the desired effects, while others may need a much smaller dose for the same results.
Although factors such as weight, age, and muscle to fat ratio are important, other factors like genetics, liver enzyme activity, underlying health conditions, digestive function, and medication use can all affect CBD supplementation.
The best way to find the right dose of CBD for your body is to start low and increase slowly over time until you achieve a dose that works for you.
Most people will start at a very low dose around 2.5 mg of CBD and increase by 2.5 mg every day until they receive the level of benefit they’re looking for. As you become familiar with how CBD works for your body, you’ll be able to adjust this dose as needed.
CBD Dosage Calculator
Tracking Your Progress
PCOS is a chronic health condition — meaning that it doesn’t appear overnight, and won’t go away overnight either. It can take months or years to improve symptoms of PCOS, so you need to be patient.
It’s difficult to see improvement in the short term for conditions like PCOS that move slowly — so it helps to keep notes of your symptoms. This way you can compare your notes over longer periods of time to spot any changes — for good or for worse.
Think of it like this — when you’re growing up, you don’t notice that you’re a little bit taller every day, yet when you compare height measurements from a year ago you may notice a big difference. It’s the same with chronic health conditions.
If you were to be asked how you feel every day, you may have the same answer — “same as yesterday”. Yet if you were to compare how you feel now, to 3 months ago, there may be a significant change — you just didn’t notice.
The best way to track your progress is to keep a journal of your symptoms. You can choose to do this every day, every few days, or even once per week.
Here are some important questions to keep in mind while tracking progress in a journal:
- What are your current symptoms?
- How would you rate each symptom on a scale of 1–10? (10 being the most severe)
- Did you have your period this month? If so, when did it start and stop?
- What foods did you eat today?
- What was your dose of CBD? Was there any noticeable improvement?
- What was your temperature upon rising in the morning? (Helpful if thyroid issues are thought to be an issue, or if you’re no longer menstruating)
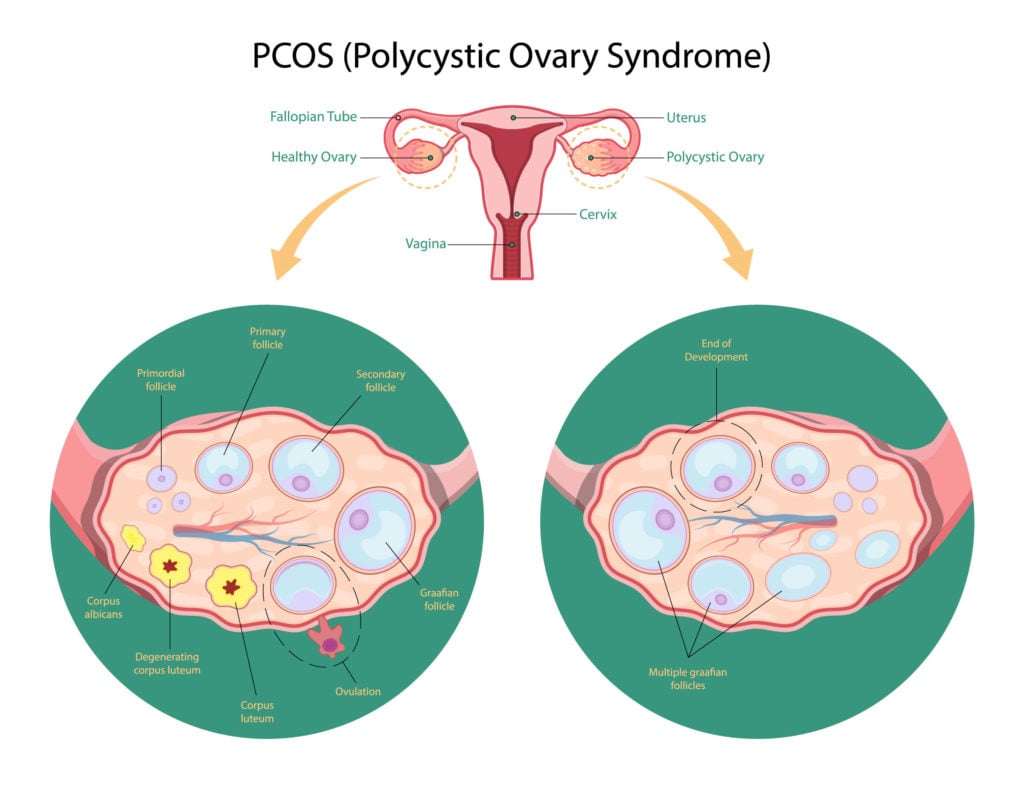
What is PCOS?
PCOS stands for polycystic ovarian syndrome. It’s a collection of symptoms (syndrome), that mimics a related syndrome called poly cystic ovarian disease (PCOD). With PCOD, visible cysts form on the ovaries — interrupting their ability to function properly.
With PCOS, these cysts aren’t visible — hence the term syndrome (set of symtpoms, but not a specific disease).
PCOS is an endocrine disorder — which means it causes a problem with hormone levels.
The most common hormones affected by PCOS is insulin, testosterone, and female reproductive hormones like estrogen, luteinizing hormone (LH), and follicle-stimulating hormone (FSH).
Related Endocrine-Related Health Conditions CBD Has Benefit Towards:
- Type II Diabetes
- Menopause (not a disorder)
- Osteoporosis
- Obesity
- Hyperthyroidism
- Hypothyroidism
- Premenstrual Syndrome (PMS)
PCOS is Not a Disease, It’s a Syndrome — What Does This Mean?
A syndrome is a collection of symptoms that occur simultaneously — often without a known cause and aren’t connected to each other. There are many different types of syndromes. An example of a syndrome you may have heard of is premenstrual syndrome — which is not a disease, but a set of symptoms.
Conversely, a disease is a specific abnormal condition that negatively affects the function of an organ or body system.
As a syndrome, there are no defining lines that group PCOS sufferers together to understand its cause and treatment. The only thing grouping them together is an overlap in the symptoms — which can vary quite a bit from one PCOS sufferer to the next.
This condition should not be confused with PCOD (polycystic ovarian disease) which has a clear cause. We’ll cover the differences between the two in more detail below.
What’s The Difference Between PCOS & PCOD?
PCOS and PCOD have similar symptoms but are very different from each other when you take a closer look.
PCOD (polycystic ovarian disease) is characterized by enlarged ovaries, usually caused by problems ejecting immature eggs from the ovaries during the menstrual cycle. This can cause the ovaries to enlarge and may begin producing excess testosterone, estrogen, or both. Many cases of PCOD have no noticeable symptoms and are only discovered by routine examination. This condition can usually be controlled by diet and lifestyle changes.
PCOS (polycystic ovarian syndrome) affects the entire body, and has a strong metabolic component and is much more severe than PCOD. With this condition, a dozen or more new cysts form in the ovaries each month. The cause of these cysts remains unknown. As cysts form, the ovaries produce more testosterone and other androgens (male hormones), which can cause dramatic changes to the body over time.
Although both conditions involve the formation of cysts in the ovaries, and changes in hormone levels — the changes involved with PCOS are much more severe. Both conditions can have a negative impact on fertility.
What Are The Symptoms of PCOS?
Only women can experience PCOS as it’s a disorder characterized by cyst formation on the ovaries (female reproductive organ). This condition can bring many symptoms, some of which seem unrelated.
Additionally, PCOS symptoms can vary a lot from one woman to the next. This makes it incredibly difficult for researchers to study the condition. PCOS in one woman could be completely different than PCOS in another woman — and likely involves a completely separate underlying cause.
Symptoms of PCOS May Include:
- Male-pattern hair growth (hirsutism)
- Acne
- Fatigue
- Headaches
- Infertility
- Mood disorders
- Pelvic pain
- Sleeping disorders
- Thinning of the hair on the head
- Weight gain
What Causes PCOS?
There’s a lot of debate about the true cause of PCOS — and the truth is that there are likely to be many different causes.
What we do know is that this condition is predominantly an endocrine disorder. Some symptoms relying on a dysfunction of the female reproductive hormones (HPO-axis), others focus more on the metabolic system (thyroid and pancreatic hormones).
All of these hormone systems rely on complex feedback loops to remain in balance. Even mild shifts in this balance can result in significant side-effects.
How does the body keep hormones in balance?
The answer is in something called a negative feedback loop — the brain tells other organs to release hormones, and only stops when it detects adequate levels of these hormones in the bloodstream (feedback).
This works in a similar way to the heating system in your house. When temperatures drop too low, the thermostat kicks the furnace on. Once it detects temperatures are within the set range, it tells the furnace to turn off again to avoid overheating the house.
If anything goes wrong during this negative feedback loop with the brain and endocrine organs (there are a lot of things that can go wrong), hormone levels can fall out of balance. This is what causes the symptoms of PCOS.
The symptoms involved with PCOS will largely rely on the endocrine organs affected.
Simplified Breakdown of Common PCOS Symptoms and Potential Causes:
| Symptom | Adrenal Glands | Pancreas | Ovaries | Thyroid Gland |
| Male-pattern hair growth | ✔ | ✔ | ||
| Acne | ✔ | ✔ | ✔ | |
| Fatigue | ✔ | ✔ | ✔ | |
| Headaches | ✔ | ✔ | ||
| Infertility | ✔ | ✔ | ||
| Mood disorders | ✔ | ✔ | ✔ | ✔ |
| Pelvic pain | ✔ | |||
| Sleeping disorders | ✔ | ✔ | ✔ | ✔ |
| Thinning of the hair on the head | ✔ | ✔ | ✔ | |
| Weight gain | ✔ | ✔ | ✔ |
PCOS & Male Hormones (Androgens)
One of the key drivers of PCOS symptoms is an excess of male hormones known as androgens.
Both men and women produce androgens like testosterone naturally. The difference is that women convert testosterone into estrogen. The most important factor is the ratio of estrogen to testosterone. In women, the ratio is heavily weighted in favor of estrogen, while men have much higher concentrations of testosterone.
With PCOS, there could be one of two problems:
- Excessive production of testosterone
- Lack of conversion into estrogen
Both result in the same thing — high testosterone levels in comparison to estrogen.
Excess androgen levels can inhibit menstruation (leading to a lack of menstruation and infertility), resulting in excess hair growth on the upper lip and back, trigger the formation of acne, and lead to changes in mood [11].
The only reliable way to find out what may be causing your symptoms is to visit a doctor.

How is PCOS Diagnosed?
If you think you may have PCOS and have not been diagnosed by a doctor, it’s important that you schedule an appointment right away.
PCOS is difficult to diagnose and is usually done through a process of elimination using advanced medical diagnostic equipment. It’s nearly impossible for someone to accurately diagnose PCOS at home.
Doctors will start with a blood test, and perform other diagnostic testing before coming to a diagnosis.
Common Tests Used to Help Diagnose PCOS:
- Fasting insulin — PCOS patients often experience hyperinsulinemia (too much insulin in the blood)
- Luteinizing hormone (LH): Follicle Stimulating Hormone (FSH) ratio — These hormones are key regulators of the female menstrual cycle. PCOS patients may have a ratio greater than 1:1 (usually around 2:1).
- SHBG levels — Sex hormone-binding globulin is often low with PCOS
- Ultrasound — This is to look for cysts on the ovaries. Cysts on the ovaries are not a confirmed diagnosis of PCOS. There are other causes for this as well.
- Thyroid Stimulating Hormone (TSH) and thyroid hormones — This is done to rule out other causes for the symptoms like hypo or hyperthyroidism.
- CRP — C-reactive protein is a good indicator of inflammation in the body, which can be used to identify other causes for the symptoms
- Full blood count — By taking a look at the concentration and size of red and white blood cells, doctors may identify other causes for the condition.
- Liver function test — In some cases, similar symptoms can be explained by problems with the liver, such as fatty liver disease.
Once the doctor has explored other options and taken family history and the patients symptoms into consideration, they’ll consider a set of criteria used to diagnose PCOS known as the Rotterdam Criteria (2003).
PCOS Diagnostic Criteria (Rotterdam Criteria)
In order to diagnose PCOS, two of the following must be identified:
- Oligoovulation and/or anovulation — ovulating less than normal or not at all
- Excess androgen activity — high concentration of male hormones in the blood
- Polycystic ovaries — multiple cysts found on the ovaries
Other endocrine disorders must be ruled out before a doctor will make a PCOS diagnosis.
Key Takeaways: Can CBD Help With PCOS?
PCOS is an endocrine disorder involving fluctuations in testosterone, estrogen, FSH, LH, and more. It can significantly affect the quality of life of those affected and remains one of the leading causes of infertility in women.
This condition has a lot of overlap with diabetes, characterized by heightened insulin levels in the blood and higher than normal male hormone production.
There are no direct studies on the effects of CBD for PCOS — but there are some speculative effects we can make from other areas of research.
The most relevant effects of CBD for PCOS involve its regulating effect on insulin levels, as well as its potential to promote weight loss and support other side-effects of the condition like anxiety.
If you’re interested in trying CBD to help manage symptoms, we highly recommend visiting your doctor first. This is important to make sure the use of CBD (or any supplement) won’t interact with any of your other medications and to assess any other factors that may interfere — such as other underlying health conditions.
More research is needed to assess the specific effects of CBD for PCOS. Stay up to date with any updates in this field of study by signing up for our newsletter below.
References Cited in This Article
- Asunción, M., Calvo, R. M., San Millán, J. L., Sancho, J., Avila, S., & Escobar-Morreale, H. F. (2000). A prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women from Spain. The Journal of Clinical Endocrinology & Metabolism, 85(7), 2434-2438.
- Weiss, L., Zeira, M., Reich, S., Har-Noy, M., Mechoulam, R., Slavin, S., & Gallily, R. (2006). Cannabidiol lowers incidence of diabetes in non-obese diabetic mice. Autoimmunity, 39(2), 143-151.
- Migrenne, S., Lacombe, A., Lefevre, A. L., Pruniaux, M. P., Guillot, E., Galzin, A. M., & Magnan, C. (2009). Adiponectin is required to mediate rimonabant-induced improvement of insulin sensitivity but not body weight loss in diet-induced obese mice. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 296(4), R929-R935.
- Sam, S. (2007). Obesity and polycystic ovary syndrome. Obesity management, 3(2), 69-73.
- Ryan, D., Drysdale, A. J., Lafourcade, C., Pertwee, R. G., & Platt, B. (2009). Cannabidiol targets mitochondria to regulate intracellular Ca2+ levels. Journal of Neuroscience, 29(7), 2053-2063.
- Scopinho, A. A., Guimarães, F. S., Corrêa, F. M., & Resstel, L. B. (2011). Cannabidiol inhibits the hyperphagia induced by cannabinoid-1 or serotonin-1A receptor agonists. Pharmacology Biochemistry and Behavior, 98(2), 268-272.
- Zuardi, A. W., Cosme, R. A., Graeff, F. G., & Guimarães, F. S. (1993). Effects of ipsapirone and cannabidiol on human experimental anxiety. Journal of psychopharmacology, 7(1_suppl), 82-88.
- Bergamaschi, M. M., Queiroz, R. H. C., Chagas, M. H. N., De Oliveira, D. C. G., De Martinis, B. S., Kapczinski, F., … & Martín-Santos, R. (2011). Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology, 36(6), 1219.
- Banerjee, S. P., Snyder, S. H., & Mechoulam, R. A. P. H. A. E. L. (1975). Cannabinoids: influence on neurotransmitter uptake in rat brain synaptosomes. Journal of Pharmacology and Experimental Therapeutics, 194(1), 74-81.
- Bakas, T., Van Nieuwenhuijzen, P. S., Devenish, S. O., McGregor, I. S., Arnold, J. C., & Chebib, M. (2017). The direct actions of cannabidiol and 2-arachidonoyl glycerol at GABAA receptors. Pharmacological research, 119, 358-370.
- Apparao, K. B. C., Lovely, L. P., Gui, Y., Lininger, R. A., & Lessey, B. A. (2002). Elevated endometrial androgen receptor expression in women with polycystic ovarian syndrome. Biology of reproduction, 66(2), 297-304.
CBD For Health & Wellness
-
Conditions Related to Health Benefits
- CBD For Allergies: Can This Cannabinoid Ease Symptoms?
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- CBD For Psoriasis: Can CBD Help to Alleviate Symptoms?
- Traumatic Brain Injury (TBI)
- Arthritis
- Anxiety & Depression
- Weight Loss
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Antibiotic Resistance
- Asthma
- Atherosclerosis
- Autism
- Acne
- Bipolar Disorder
- Pain
- Crohn's Disease & Ulcerative Colitis
- Diabetes
- Epilepsy
- Endocrine Disorders
- Fibromyalgia
- Fatty Liver Disease
- Glaucoma
- Hypertension
- Heart Disease
- Huntington's Disease
- Inflammation
- Irritable Bowel Syndrome (IBS)
- Kidney Disease
- Migraine Headaches
- Muscle Recovery
- Multiple Sclerosis
- Motion Sickness
- Metabolic Syndrome
- Neurodegeneration
- Cancer
- Nausea
- Neuropathic (Nerve) Pain
- Osteoporosis/Bone Health
- Obsessive-Compulsive Disorder (OCD)
- Polycystic Ovarian Syndrome (PCOS)
- PTSD
- Prion/Mad Cow Disease
- Premenstrual Syndrome (PMS)
- Parkinson’s Disease
- Schizophrenia
- Sickle Cell Anemia
- Stroke
-
Conditions Related to Products
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 10 CBD Oils For Back Pain
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Terpene Concentrates
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- Best Dry Herb Vaporizers
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
Conditions Related to Topicals
-
Conditions Related to Oils & Tinctures
-
Conditions Related to Edibles
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Honey
- CBD Chewing Gum
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Coffee
- CBD Drinks & Shots
- CBD Capsules
-
Conditions Related to Gummies
- Ranking The Top 13 THC Gummies By Category (Δ8, Δ9, Δ10, HHC, & More)
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
-
Conditions Related to Hemp Flower
-
-
Conditions Related to Terpenes
-
-
Conditions Related to Cultivation
-
Conditions Related to Concentrates
-
Conditions Related to Delta 8 THC
-
Conditions Related to Delta 9 THC
-
-
-
-
Conditions Related to CBD
- Everything You Need to Know About CBD Sunscreen
- Top 7 CBD Gummies For Sleep & Insomnia
- Top 7 CBD Gummies To Help With Anxiety (2022)
- Best CBD Gummies For Pain (Top-Rated Pain Gummies For 2022)
- Best Hemp Cigarettes (Top 5 Nicotine-Free Smokes)
- Top 5 CBD Lip Balms For 2022
- The Top 7 CBD Face Masks for 2022
- The Best CBD Inhalers For 2022 (& How to Use Them)
- Best Full-Spectrum CBD Vape Juice: What to Look For & How to Use It
- CBD Eye Drops: New Option For Glaucoma?
- CBD Oil For Dogs With Arthritis
- Best CBD Massage Oils In 2022
- Buyer's Guide To The Best CBD Vape Kits In 2022
- CBD Chocolate: Yes, It Exists & It's Just as Divine as it Sounds
- CBD Pre-Rolls & Cigarettes
- Best CBD Soaps
- Best CBD Shampoo & Conditioner
- Best CBD Juul Pods
- CBD Isolate Oils
- Full-Spectrum CBD Oils
- Best CBD Lube
- CBD Honey
- CBD Transdermal Patches
- CBD Oil For Dogs With Epilepsy
- CBD Oil For Dogs With Anxiety
- CBD Oil For Dogs With Cancer
- CBD For Horses
- CBD Chewing Gum
- CBD Pain Cream
- CBD Oil For Cats
- CBD Oil For Dogs
- CBD Hemp Flower
- CBD Suppositories
- Best CBD Gummies for Pain, Sleep & Anxiety Reviewed (2022)
- CBD Teas
- CBD Vape Pens
- CBD Vape Oils
- CBD Coffee
- CBD Drinks & Shots
- CBD Crystals
- CBD Skincare
- Best CBD Oil & Gummies For Kids: Is CBD Safe for Children with Anxiety & ADHD?
- CBD Concentrates
- CBD Bath Bombs
- CBD Capsules
- CBD Sprays
- CBD Dog Treats
-
-
Conditions Related to THC-O
-
-
Conditions Related to Joint Health
-
Conditions Related to Pain Disorders
- Top 10 CBD Oils For Back Pain
- Can CBD Help With Menstrual Cramps?
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Traumatic Brain Injury (TBI)
- Arthritis
- Pain
- Fibromyalgia
- Glaucoma
- Inflammation
- Kidney Disease
- Migraine Headaches
- Multiple Sclerosis
- Neuropathic (Nerve) Pain
- Premenstrual Syndrome (PMS)
- Sickle Cell Anemia
-
Conditions Related to Autoimmune Disease
-
Conditions Related to Cognitive Health
-
Conditions Related to Metabolic Disorders
-
Conditions Related to Psychological Disorders
-
Conditions Related to Muscles & Bones
-
Conditions Related to Nervous System
- CBD for Sciatica: How It Works, Safety, Drug Interactions, & Best Products
- Is CBD a Viable Treatment for Cerebral Palsy?
- CBD Oil For Sleep
- Traumatic Brain Injury (TBI)
- Anxiety & Depression
- ADD & ADHD
- Anorexia
- Alzheimer’s Disease & Dementia
- Addiction
- ALS (Amyotrophic Lateral Sclerosis)
- Autism
- Bipolar Disorder
- Epilepsy
- Huntington's Disease
- Inflammation
- Migraine Headaches
- Multiple Sclerosis
- Motion Sickness
- Neurodegeneration
- Neuropathic (Nerve) Pain
- Obsessive-Compulsive Disorder (OCD)
- PTSD
- Prion/Mad Cow Disease
- Parkinson’s Disease
- Schizophrenia
-
-
Conditions Related to Reproductive Health
-
Conditions Related to Hormones & Endocrine
-
Conditions Related to Skin Health
-
Conditions Related to Cardiovascular System
-
Conditions Related to Digestive System
-
Conditions Related to Genetic Disorders
-
Conditions Related to For Children